The American Cancer Society estimates more than 281,550 new cases of breast cancer will be diagnosed in the United States in 2021 and an estimated 43,600 patients will not survive the disease.1 Identifying patients at increased risk for developing breast cancer allows them to take control of their healthcare and reduce their risk.1 In the US population, there are 32 million patients (10%) with a concerning family history, for whom medical management could reduce their risk of developing breast cancer.2 A pathogenic variant causes approximately 10% of breast cancers. One million patients are carriers, yet 95% of patients have yet to be tested.2
The United States Preventive Services Task Force recommends primary care providers screen patients who have a concerning personal or family history of breast or ovarian cancer.3 The National Comprehensive Cancer Network (NCCN) recently provided an update with the latest evidence-based recommendations for screening, genetic counseling/testing, and management for patients who are at high risk for breast cancer or who have been diagnosed with hereditary breast and ovarian cancer syndrome (HBOC).4 These recommendations serve as a guide for providers to direct appropriate high-quality patient care that leads to improved patient outcomes.
Project purpose
The purpose of this quality improvement (QI) project was to develop and implement an HBOC risk assessment protocol in a primary care setting using NCCN guidelines. The goal of the project was to facilitate provider utilization of NCCN guidelines for improved patient outcomes. The project aims were in keeping with those identified by the Institute of Medicine (now US Health and Medicine Division) in 2001 to facilitate services that are effective, patient centered, timely, and efficient.5
Setting/population
The setting for the project was a private practice medical clinic that provides women’s health services to patients who are mostly between the ages of 25 and 64 years. Over 90% of patients have private insurance, but the clinic accepts Medicare. All healthcare providers, staff, and patients who met the inclusion criteria were invited to participate in the QI project. The inclusion criteria were met if the patient’s personal or family history was concerning for HBOC based on NCCN guidelines. Missouri State University institutional review board approved the QI project. Informed consent was required prior to participation.
Description of the quality improvement project
The need for this project was identified at staff meetings during which gaps in identifying patients at risk for HBOC were acknowledged. A consensus was reached to develop and implement an evidence-based approach to assessing patients for HBOC risk. Prior to this project, cancer family history was being collected on occasion. NCCN guidelines were not being followed due to a lack of provider’s knowledge regarding HBOC. Six objectives were used to guide the development, implementation, and evaluation of the project.
Objective 1 was to increase healthcare provider and staff’s knowledge about NCCN recommendations. Healthcare provider and staff education included presentations at the monthly staff meeting that lasted an hour. The educational sessions occurred over a 4-month time frame. Aims for this objective were to have 90% of healthcare providers and staff attend in-office educational sessions and to demonstrate a 10% knowledge improvement.
Objective 2 was to increase patient knowledge about genetic mutations, risk and benefits of genetic testing, and medical management considerations based on risk of HBOC. The aim was for patients who attended a genetic counseling appointment to have a 10% knowledge improvement.
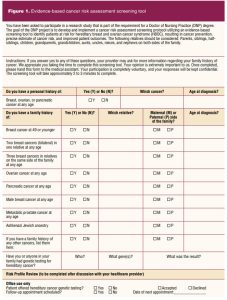
Objective 3 was to develop and implement an HBOC risk assessment protocol utilizing an evidence-based screening tool to identify patients at risk and a multidisciplinary approach in the management of and recommendations for these patients. The protocol included clear primary, secondary, and tertiary referral mechanisms for staff to follow. The aims for this objective were to have 100% of patients referred to primary, secondary, and tertiary care as appropriate. The evidence-based screening tool was developed based on NCCN criteria for patients at risk for HBOC (Figure 1). The screening tool was given to patients during the check-in process.
Objective 4 was to implement a follow-up appointment protocol after the patient’s genetic testing appointment. The aim for this objective was to have 90% of patients seen within 2 to 3 weeks following their initial genetics consultation to have their genetic results disclosed.
Objective 5 was to develop a protocol within the electronic health record (EHR) to track patients who are at risk for HBOC. The aim for this objective was to capture all patients who met NCCN criteria as high risk for possible HBOC.
Objective 6 was to provide all staff at the clinic with access to supporting tools such as educational materials about HBOC, protocol checklists, EHR internal referral and order sets, decision support systems, standardized patient information leaflets, and documentation templates within the EHR.
Methods to evaluate outcomes
Recording of the number of healthcare providers and staff attending the educational sessions and pre-and post-session surveys were utilized to evaluate project objective 1. A 20-item survey was used to evaluate the healthcare provider and staff’s knowledge of cancer risk assessment, genetic testing, and management strategies recommended by NCCN prior to and after the educational sessions. A reliability analysis was computed to determine the psychometric properties for the understanding subscales and was performed using Cronbach’s alpha. The patient understanding subscale Cronbach’s alpha was .94 and staff understanding subscale was .92; thus both were reliable. For objective 2, patients completed pre-and post genetic counseling appointment surveys to evaluate changes in knowledge. All data for the pre and post surveys were entered into JASP software for analysis. Demographic data obtained from the patient surveys were also reviewed.
Clinical aggregate data were extracted from the EHR to evaluate outcomes for objectives 3 to 5. Pre-and post-protocol implementation data on referrals of patients at risk for HBOC to primary, secondary, and tertiary care centers; number of patients seen in the clinic within 2 to 3 weeks following genetic testing appointment for results; and percentage of patients at risk for HBOC identified by the evidence-based screening tool were obtained. Objective 6 was evaluated by a review of the EHR to determine presence of supporting tools. Comparisons of all pre-and postimplementation data were calculated using a dependent sample t-test. Results for all evaluation methods were calculated using descriptive statistics such as frequencies and percentages.
Outcomes
A total of 64 patients were enrolled in the QI project over a 4-month period. The age range was from 25 to 65 years or more, with the majority (42%) between age 45 and 54 years. The majority (92%) of patient participants identified as female. A total of eight providers and staff (100%) participated in the project. All participating staff, providers, and patients completed the pre-and post-educational session surveys. As an aggregate, knowledge scores increased from 80% to 100% for providers, staff, and patients. This represented a 25% increase exceeding the aim of a 10% increase. Additional items on the patient survey revealed that 57% of patients had disclosed their cancer family history to a medical provider in the last year and 88% of patients identified as high risk for HBOC had not been offered genetic testing in the past by their medical provider.
All participating patients were seen within 2 to 3 weeks after their initial genetics consultation to have their genetic test results disclosed exceeding the 90% aim. Prior to implementation of the protocol, 60% were seen within 2 to 3 weeks. The system metrics within the EHR tracked 100% of patients who were identified as at risk for HBOC. Supporting tools for staff were identified in the EHR.
During the project, there were six positive genetic mutations identified, which correlated to a 9% positive mutation rate. The genetic mutations identified were PALB2, NTHL1, BRCA2, and MUTYH. Medical management recommendations changed for 28% of the project participants who were genetically negative but high risk based on their familial risk of cancer.
Discussion
Barriers
One of the barriers for this QI project was the cancer family history collection. Often, patients were unsure of the origin of the cancer or age at diagnosis. The barrier was mitigated by allowing extra time for the participant to call a family member and adequate time to complete the cancer risk assessment tool. It would be more informative and accurate if the patient was able to collect the cancer family history prior to their appointment.
Facilitators
The QI project had two main facilitators. The first facilitator was the office manager of the clinic. She supervised the receptionists and made sure the project workflow was being followed (Figure 2).

The second facilitator was the lead medical assistant who helped on the clinical side of the QI project. She also managed the referrals between secondary and tertiary centers.
Lessons learned
The project director learned that you can never predict what DNA is doing. Over the duration of the project, there were certain family histories that strongly suggested genetic mutation, but these typically were not the patients with a newly diagnosed genetic mutation. The participants with genetic mutations that were identified in the QI project had a more subtle family history. A next step in this clinic site is to develop metrics for tracking patients within their EHR who require close follow-up due to either genetic mutation status or familial risk.
Implications for practice
Capturing a cancer family history is a significant component in providing comprehensive care. Family history provides the key psychosocial and medical risk information needed to appropriately manage the care of patients. Education and an HBOC risk assessment protocol with necessary tools and resources can facilitate provider consistent use of NCCN guidelines in clinical practice. As demands grow for providers to increase productivity while providing quality care, developing protocols to provide efficient yet evidence-based and patient-centered care is critical to improving patient outcomes.
Sustainability
Several factors indicate that this project is sustainable at this clinic. The project is in line with the clinic’s mission built around the support of evidence-based practice. The entire staff has been highly receptive to the initial implementation and continuation of the protocol. The project has low overhead and the potential to increase revenue for the clinic long term based on increased patient visits and new referrals generated from community outreach efforts.
Limitations
Limitations include the short-time interval for data collection and small sample size. Outcome evaluation could be enhanced with a longer implementation period with increased numbers of participants.
Conclusion
The development and implementation of an HBOC risk assessment protocol can decrease morbidity and mortality. NCCN guidelines are available to assist providers in all aspects of protocol development. Evaluation tools should be utilized to monitor outcomes so there can be continuous improvement in implementation.
Rachel M. Fidino is CEO of New U Women’s Clinic & Aesthetics in Kennewick, Washington. Melissa R. Penkalski is Graduate Program Director at Missouri State University in Springfield, Missouri. The authors have no actual or potential conflicts of interest in relation to the contents of this article.
Acknowledgments: We thank the staff, patients, and providers for their support and participation in this project.
References:
- American Cancer Society. About breast cancer. 2021.
- Frieder R, Kendig S. Hereditary cancer testing in a value based world: the evolving standard of care. 2016.
- US Preventive Services Task Force. Final recommendation statement. BRCA-related cancer: risk assessment, genetic counseling, and genetic testing. August 19, 2019.
- National Comprehensive Cancer Network. Genetic/familial high-risk assessment: breast and ovarian. 2019.
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.

