NPWH believes a need exists for extensive research to better understand modifiable factors that influence brain health, improve one’s ability to make an early diagnosis of CI, establish effective therapies to prevent and treat CI, and support families and caregivers of individuals with CI. NPWH endorses federal and state policies that devote resources to finance the needed research and that ensur e access to needed diagnostic, care, and treatment resources for individuals with CI, caregivers, families, and healthcare providers.
Background
Cognitive function refers to memory, speech, language, judgment, reasoning, and planning and thinking abilities.1 Brain health is a term commonly used to describe healthy cognitive function.2,3 Changes in these functions may indicate CI. These changes may range in their level of severity, may be progressive, and may have treatable causes.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition’s (DSM-5’s) diagnostic categories of minor and major neurocognitive disorders (NCDs) reflect the range in CI severity. Minor NCD is a condition in which the individual has mild but measurable changes in cognitive function that are noticeable to the person affected and to family members and friends but do not affect the individual’s ability to carry out activities of daily living (ADLs).1 Minor NCD may be progressive. Approximately 15%-20% of persons aged 65 years or older have minor NCD.4 Major NCD is impairment characterized by decline in at least two cognitive domains (e.g., memory, attention, language, visuospatial function, executive function) severe enough to affect a person’s ability to perform ADLs; the individual also may exhibit behavioral and psychological symptoms.1 Dementia is a commonly used term for major NCD.
Alzheimer’s disease (AD), a progressive degenerative brain disease, is the most common cause of dementia.1 Most statistics on dementia reflect data related to AD. As of 2018, about 5.7 million adults in the United States have AD, with 5.5 million of them being aged 65 years or older. As the size and proportion of this older U.S. population grows, it is projected that 7.1 million persons aged 65 or older will have dementia, primarily AD, by 2025.1 The annual number of new cases of AD and other dementias will likely double by 2050 unless research discovers the key to prevention.1
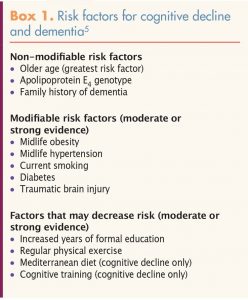 These statistics do not reflect pre-clinical AD. Current thinking is that Alzheimer’s-related brain changes may begin 20 or more years before symptoms occur.1 No proven strategies are available to prevent AD. However, recognized risk factors for cognitive decline and AD, some modifiable, do exist.5,6 Increasing evidence suggests that lifestyle interventions may have a long-term impact on preserving brain health. The Alzheimer’s Association published a report in 2015 summarizing existing evidence related to risk factors and risk reduction (Box 1).5
These statistics do not reflect pre-clinical AD. Current thinking is that Alzheimer’s-related brain changes may begin 20 or more years before symptoms occur.1 No proven strategies are available to prevent AD. However, recognized risk factors for cognitive decline and AD, some modifiable, do exist.5,6 Increasing evidence suggests that lifestyle interventions may have a long-term impact on preserving brain health. The Alzheimer’s Association published a report in 2015 summarizing existing evidence related to risk factors and risk reduction (Box 1).5
All nurse practitioners (NPs) who care for midlife and older adults play a critical role in early recognition of CI. Early signs and symptoms include problems with memory or language, noted deficits in personal or instrumental ADLs, and concerns reported by the individual or a family member or caregiver.7-9 Assessment to detect CI is a required component of the annual wellness visit established in 2011 for Medicare recipients under the Patient Protection and Affordable Care Act.7
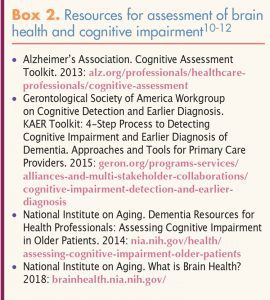
The Alzheimer’s Association has published guidance on detection of CI during the annual wellness visit. This guidance includes an algorithm for health risk assessment, patient observation, unstructured questioning, and structured assessment.7 Use of a structured cognitive assessment instrument can improve detection of CI in primary care settings by identifying individuals who may need further evaluation. Validated brief cognitive assessment tools that can be administered in 5 minutes or less in the primary care setting are available. Individuals whose assessment findings indicate possible CI should be evaluated further or referred to a specialist.7 Several initiatives have provided lists of these assessment tools, as well as recommendations and strategies NPs can use to address brain health and CI (Box 2).10-12
 Early detection of CI and diagnosis of dementia are integral to individual and family counseling, advance care planning, and consideration of supportive therapies.13-15 The years from diagnosis to end-of-life may be fraught with poor health and disability, resulting in loss of independence and, over time, a substantially lowered quality of life. When interprofessional team members work together with the individual, family members, and caregivers, the changes that occur throughout the course of the disease process can be anticipated and the best care provided.
Early detection of CI and diagnosis of dementia are integral to individual and family counseling, advance care planning, and consideration of supportive therapies.13-15 The years from diagnosis to end-of-life may be fraught with poor health and disability, resulting in loss of independence and, over time, a substantially lowered quality of life. When interprofessional team members work together with the individual, family members, and caregivers, the changes that occur throughout the course of the disease process can be anticipated and the best care provided.
The impact of this disease on quality of life extends to the more than 16 million adults in the U.S. who provide unpaid care for loved ones with dementia.1 Approximately two-thirds of these informal caregivers—that is, 10.7 million of them—are women, and more than one-third of these women are the daughters of the individuals with dementia.1 The average age of caregivers is 49 years, although about one-third of them are aged 65 years or older.1,16 One-fourth of caregivers belong to a sandwich generation—that is, they are caring not only for an aging parent but also for children younger than age 18.1
Caregiving tasks include helping with instrumental ADLs (e.g., shopping, providing transportation, managing finances) and personal ADLs (e.g., bathing, dressing, feeding). In addition, caregivers may coordinate healthcare and support services. As dementia progresses, caregivers often must manage behavioral symptoms of the disease (e.g., aggressive behavior, wandering).1 Such tasks can take an emotional and physical toll on caregivers, as well as affect their financial status if they must modify or terminate paid employment and pay for healthcare services for themselves and their care recipient.1,16 In many cases, their own needs go unrecognized and unattended.15
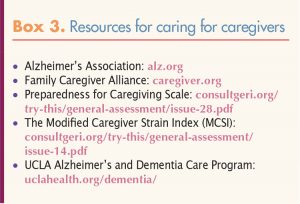 A call to action has arisen to transform policies and practices affecting the role of informal caregivers as a major source of care for a growing population of older adults with dementia. A strategic national-level action plan will be required to address the needs of these caregivers. Policies to create evidence-based training for informal caregivers specific to the care of individuals with dementia, provide support such as expanded family leave and job protection for working caregivers, and fund evidence-based caregiver services are critical. Policies must recognize the needs and values of a diverse population of caregivers and the individuals under their care.15,17,18 Box 3 lists resources devoted to caring for caregivers themselves.
A call to action has arisen to transform policies and practices affecting the role of informal caregivers as a major source of care for a growing population of older adults with dementia. A strategic national-level action plan will be required to address the needs of these caregivers. Policies to create evidence-based training for informal caregivers specific to the care of individuals with dementia, provide support such as expanded family leave and job protection for working caregivers, and fund evidence-based caregiver services are critical. Policies must recognize the needs and values of a diverse population of caregivers and the individuals under their care.15,17,18 Box 3 lists resources devoted to caring for caregivers themselves.
Implications for women’s healthcare and NP practice
Nurse practitioners who provide healthcare to women of all ages have the opportunity to address brain health during annual well-woman visits and/or during other visits if concern about patients’ cognitive function arises. In addition, NPs are likely to see, on a regular basis, a large portion of the roughly 10.7 million informal caregivers who are female. NPs are in an excellent position to identify women who are in the caregiver role and address their physical and mental health needs, including their brain health needs.
Recommendations
Nurse practitioners who provide healthcare for mid-life and older women, as well as women of any age who may be caregivers for loved ones with dementia, should:
- raise the topic of brain health as part of women’s health during routine healthcare visits;
- address risk factors for cognitive decline that may be reduced with lifestyle changes (e.g., improved nutrition, regular physical activity, cognitive training, smoking cessation);
- include a question about memory or cognition on health risk questionnaires;
- observe for signs and symptoms of CI;
- use an evidence-based protocol for screening and diagnostic evaluation of patients’ brain health and referral for further evaluation if indicated;
- include a question about any caregiving responsibilities in health assessment;
- offer additional screening for caregivers to assess preparedness for caregiving and caregiver strain;19,20
- develop health system partnerships to connect individuals with dementia and their caregivers with community agencies to identify needs and access help;
- collaborate with affected individuals, caregivers, and an interprofessional team to facilitate decision making and planning (e.g., living arrangements, advance care planning, end-of-life care) that addresses changing needs over time and across care settings; and advocate for policies at local, state, and national levels that address the needs and values of individual with dementia and their caregivers.
NPWH will provide leadership to ensure that:
- continuing education programs and other evidence-based resources are available for NPs to learn and update knowledge regarding brain health, dementia, and caregiver needs;
- ongoing collaborative engagement occurs with a variety of stakeholders to address brain health and caregiving issues as important components of an older women’s health agenda;
- research moves forward in all aspects of brain health to prevent dementia, treat existing CI, help those with CI maintain function and quality of life, and support caregivers; and
- policies strongly support individuals and families in coping with the physical, emotional, and financial burden of dementia.
References
- Alzheimer’s Association. 2018 Alzheimer’s Disease Facts and Figures. alz.org/alzheimers-dementia/facts-figures
- Alzheimer’s Association. Brain Health. 2018. alz.org/help-support/brain_health
- National Institute on Aging. What is Brain Health? 2018. brainhealth.nia.nih.gov/
- Roberts R, Knopman DS. Classification and epidemiology of MCI. Clin Geriatr Med. 2013;29(4):753-772.
- Baumgart M, Snyder HM, Carrillo MC, et al. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimers Dement. 2015;11(6):718-726.
- Moga D, Roberts M, Jicha G. Dementia for the primary care provider. Prim Care Clin Office Pract. 2017;44(3):439-456.
- Cordell CB, Borson S, Boustani M, et al. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement. 2013;9(2):141-150.
- Falk N, Cole A, Meredith TJ. Evaluation of suspected dementia. Am Fam Physician. 2018;97(6):398-405.
- Scott J, Mayo A. Instruments for detection and screening of cognitive impairment for older adults in primary care settings: a review. Geriatr Nurs. 2018;39(3):323-329.
- Alzheimer’s Association. Cognitive Assessment Toolkit. 2013. alz.org/professionals/healthcare-professionals/cognitive-assessment

