This study was conducted to describe the education, comfort, and perceived competency of a group of nurse practitioners and midwives who provide perinatal care to women with disabilities. The results are presented and the implications discussed.
Approximately 8 million women of reproductive age report having a disability.1,2 Studies have shown that women with disabilities give birth at rates similar to those of women without disabilities.3-5 Among women with a disabling condition, 51% report being physically disabled, 30% report a mental or developmental disability, and 19% report a sensory disability.6
Regardless of the type of disability, many affected women have limited access to healthcare, resulting in unmet reproductive healthcare needs.7-10 Furthermore, studies suggest that some healthcare providers (HCPs) caring for women lack sufficient knowledge about disabilities, as well as harbor negative stereotypes about the sexuality and the reproductive capability of women who have a disability.3,8,11-13
Definitions
The term disability has medical, legal, and social definitions.
Medical
 The CDC defines disability as a condition that impedes activity and the ability to participate in daily activities.2 The World Health Organization (WHO) defines disability as a complex phenomenon that includes impairments, activity limitations, and restrictions on participating in daily life because of one’s body function or structure.14
The CDC defines disability as a condition that impedes activity and the ability to participate in daily activities.2 The World Health Organization (WHO) defines disability as a complex phenomenon that includes impairments, activity limitations, and restrictions on participating in daily life because of one’s body function or structure.14
Disabilities are classified as physical, sensory, neurologic, and/or developmental. Many individuals with one or more types of disability have co-morbid conditions related to the disability or disabilities. Physical disabilities include those occurring from birth (e.g., spina bifida), those caused by trauma (e.g., spinal cord injury), and those related to a health condition (e.g., cancer and/ or its treatment). Sensory disabilities include those involving vision (e.g., myopia), hearing, smell, taste, or tactile perception. Neurologic and developmental disabilities include those that occur during fetal development (e.g., microcephaly), birth (e.g., anoxia), or exposure to toxic substances (e.g., alcohol, lead). Developmental disabilities include spectrum disorders (e.g., autism) and cognitive delays/deficits (e.g., intellectual disability).
Legal
The Americans with Disabilities Act (ADA), enacted in 1990, defines disability as a physical or mental impairment that substantially limits one or more major life activities of an individual, a record of such an impairment, and being regarded as having such an impairment.15 The ADA requires reasonable accommodations for patients with disabilities, including access to public services and HCPs.15
Social
According to the Social Model of Disability, people are disabled by barriers (physical or attitudinal) in society, not by their impairment or diff erences.16,17 The Social Model explores and supports the needs of persons with disabilities, as opposed to the limits that a disability may incur. The social defi nition of disability is based not on medical or legal terms but, rather, on an attitudinal construct. Many women with disabilities consider themselves healthy and want to be viewed that way. They need assistance from HCPs to support their health goals, which may include pregnancy.
Review of the literature
Women who have disabilities face social and environmental barriers that increase their risk for experiencing health disparities. Decreased access to high-quality care may lead to lower rates of screening for cervical and breast cancers, as well as unmet sexual and reproductive healthcare needs.3,6,9
Multiple studies have explored the experiences of women with disabilities as they access and receive perinatal care.1,3,7,8,10-12 In a qualitative study, female participants with a physical, sensory, and/or intellectual disability (N = 17) welcomed pregnancy as an experience that would affi rm their identity and worth as women and as mothers.18 However, these same participants reported that their HCPs lacked suffi cient knowledge about disabilities and their impact on pregnancy. They reported a lack of support from their HCP for their goal of motherhood, coupled with a perceived expectation of failure and an unnecessary categorization of themselves as women with high-risk pregnancies. Furthermore, participants reported that postpartum care focused mainly on the infant, and that any attention paid to them was from the perspective of what they weren’t able to do rather than what they were able to do. Participants reported that threats were made to remove their infant from the home if the care they provided to their infant was assessed as suboptimal.
Mitra et al8 interviewed 25 women with a physical disability who had given birth within the past 10 years. Participants reported that physicians and nurses providing perinatal care demonstrated a lack of knowledge and a poor attitude about pregnancy among women with disabilities. In addition, participants reported a lack of assistive devices in the healthcare setting.
In a study focused on the provider’s point of view, Smeltzer et al19 interviewed 14 HCPs—13 physicians and 1 certified nurse-midwife (CNM)—who reported providing care to women with physical disabilities. The investigators found that none of the HCPs reported having formal education or training on how to provide care to women with disabilities during the perinatal period. However, all of them reported having a positive attitude and found the experience rewarding.
The study
Nurse practitioners (NPs) and CNMs are instrumental in providing care during the perinatal period to women with disabilities. However, little is known about the educational preparation, comfort, perceived competency, and practice challenges of NPs and CNMs in delivering perinatal care to this population. The purpose of this study was to describe the education, comfort, perceived competency, and practice challenges of NPs and CNMs in the provision of perinatal care to women with disabilities.
Methods
The authors developed a 37-item survey to describe the provision of perinatal care to women with disabilities by these HCPs. Two questions measured recall of educational exposure to disability content and one question ascertained whether participants felt that their education about disabilities was suffi cient for practice. Nine questions measured respondents’ comfort in providing care to women with disabilities. The concept of practitioner comfort in care delivery has been linked to improved healthcare outcomes and patients’ sense of being respected.20,21 Ten questions assessed perceived competency in providing healthcare to women with disabilities. In addition to completing the survey, respondents had an opportunity to provide narrative comments on challenges they faced when providing care to women with disabilities. The remaining questions pertained to demographic data collection.
Prior to distribution, the survey underwent expert review by three advanced practice registered nurses (APRNs), including one CNM, for readability, content, and face validity. Minor changes were made to the survey to clarify the questions. After approval by the institutional review board, the survey was distributed by email to the membership of a leading APRN organization (N = 2,400) using SurveyMonkey. The letter accompanying the survey instrument served as consent. All data were collected anonymously. Members currently practicing as NPs or CNMs were invited to take the survey. Student members, as well as NPs and CNMs not currently practicing, were ineligible to participate. Data were collected between October 2015 and December 2015.
Frequencies and percentages were used to examine the distribution of responses. Chi-square (χ2) statistics were used to test associations among education, comfort, competency, and demographic variables. Statistical tests were considered signifi cant at an alpha of .05. The Cronbach alpha for the survey instrument was 0.92 overall. Data were analyzed using SPSS version 24.
Results
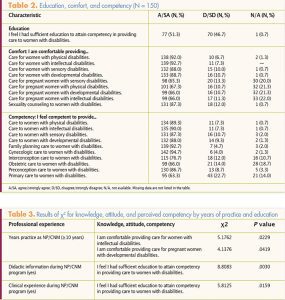
Of the 2,400 surveys emailed, 185 were returned (response rate, 7.8%); of the 185 surveys returned, 150 were eligible for inclusion in the fi nal analysis (final response rate, 150/2,400, or 6.25%). Table 1 provides respondents’ demographic data and education and practice histories. Table 2 lists their levels of education, comfort, and competency in caring for women, including pregnant women, with disabilities.

A significant relationship existed between professional experience (years of education and practice) and educational preparation, comfort, and perceived competency in providing care to women with disabilities (Table 3). NPs/CNMs in practice <10 years reported greater perceived competency providing care to pregnant women with intellectual (χ2 = 5.18, n = 150, P <.05) or developmental (χ2 = 4.14, n = 150, P <.05) disabilities. In addition, NPs/ CNMs who received didactic (χ2 = 8.81, n = 150, P <.001) or clinical (χ2 = 5.81, n = 150, P <.05) education in this area were more likely to feel that they received sufficient education to attain competency in providing care to women with disabilities than did those who reported receiving none of this content.
Respondents’ narrative comments focused on challenges delivering perinatal care to women with disabilities, including inadequate time to provide care, limited access to assistive devices, few referral resources for consultation, communication challenges, and lack of guidelines for care provision. Physical challenges pertained primarily to physical space and equipment—or the lack thereof. Respondents reported a lack of equipment to provide adequate care for patients with physical disabilities or mobility impairments. For example, many reported that their workplace had only one examining table that could be lowered enough to accommodate a woman with a physical disability, resulting in delays in seeing patients if the room with this usable table was occupied.
Communication was the primary challenge when caring for women with sensory disabilities. In particular, working with hearing-impaired patients was diffi cult without an interpreter, profi ciency in sign language, or another way to communicate eff ectively with them. Some respondents reported not having adequate educational materials for visually impaired/blind patients.
Provider-specific challenges addressed individual concerns about being prepared to meet the needs of women with disabilities. Some respondents noted that they did not feel adequately informed about specifi c conditions or how those conditions aff ected pregnancy or general health. Others noted diffi culty in keeping up to date with recommendations, guidelines, and regulations related to disabilities.
Overall, respondents felt that time constraints were a major challenge when providing care to women with disabilities.
Limitations
The low response rate must be acknowledged. The survey was distributed electronically to members of a national organization that represents APRNs who specialize in women’s health. Some email addresses may not have been active or emails may not have been properly delivered or received. Reminder emails were sent 2 weeks after the initial request. To increase response rates in future studies, researchers might consider off ering an incentive such as a gift card. Another option is to conduct the study at the member organization’s annual conference. The authors are unable to comment or speculate on the delivery of perinatal care that survey non-responders provide to women with disabilities. Generalizability to all APRNs might not be possible because of the low response rate.
Box. Educational resourcesAmerican College of Obstetricians and Gynecologists. Women with Disabilities. 2017. acog.org/About-ACOG/ACOG-Departments/Women-with-Disabilities Byrnes L, Hickey M. Perinatal care for women with disabilities: clinical considerations. J Nurse Pract. 2016;12(8):503-509. sciencedirect.com/science/ article/pii/S1555415516303002 Center for Research on Women with Disabilities. bcm.edu/research/centers/research-on-women-with-disabilities CDC. Disability and Health. Women with Disabilities. cdc.gov/ncbddd/ disabilityandhealth/women.html |
Discussion and clinical implications
Although most survey respondents did not receive formal education or training in providing perinatal care to women with disabilities, this group reported feeling competent and comfortable in delivering such care. The authors ascribe these feelings to respondents’ experience levels. The authors did not ask respondents whether they sought learning opportunities in the form of continuing education (CE) programs or conferences on providing care to women with disabilities. This inquiry is an important consideration for future research, as well as for program development.
The overwhelming majority of respondents reported seeing fewer than 10 patients with a disability per month. This fi nding may be consistent with the data on limited access to and use of healthcare services, particularly reproductive health services, on the part of women with disabilities.3,6
Fewer than 30% of respondents reported having assistive devices and/or equipment to facilitate care in their clinical practice setting, which may present an actual or potential barrier to utilization of care by women with disabilities. According to the ADA, facilities, including healthcare facilities, are required to have accommodations and be accessible to persons with disabilities. Access and accommodations include transportation, ease of maneuverability within the physical space, and appropriate equipment.
Given the estimate of the number of women with disabilities in the population, many are likely not receiving the care they need. Provision of comprehensive care by competent, sensitive HCPs is necessary; however, accomplishing this goal presents challenges. A comprehensive overview of providing perinatal care to women with disabilities is available with CE credit.22 As noted in the current survey, HCPs are not routinely educated on the unique care needs of persons with disabilities. This fi nding is consistent with those of Smeltzer et al19 regarding obstetrical care providers. The Box lists and provides links to educational resources for practitioners and students alike. These resources can be incorporated into existing course work.
Environmental accommodations for patients with disabilities are costly and not necessarily easily implemented. Many HCPs may be unaware of resources and referrals within their geographic location, perhaps because of the limited number of patients they encounter who require these services. Most important, the substantial time required to deliver appropriate, comprehensive care tends not to be allocated in scheduling. HCPs should have not only the necessary physical accommodations for patients with disabilities but also the knowledge about how each disability can aff ect health during the perinatal period and in general.
Advanced practice registered nurses can help bridge the gaps in care and help ensure favorable experiences with the healthcare system. Raising awareness about the unique needs of women with disabilities is one step toward ensuring a more positive experience for them.
Lorraine Byrnes is Associate Professor, Mary Hickey is Clinical Professor, Jin Young Seo is Assistant Professor, and Lorie Goshin is Assistant Professor, all at Hunter Bellevue School of Nursing, Hunter College, City University of New York. The authors state that they do not have a fi nancial interest in or other relationship with any commercial product named in this article.

