Cancer is the second leading cause of death in the United States, with colorectal cancer being the third most common type of cancer in women and men. In 2018, colorectal cancer was the third leading cause of cancer-related deaths in women, with 32 new cases reported for every 100,000 women.1 The 5-year relative survival rate for all Surveillance, Epidemiology, and End Results (SEER) program stages combined for those diagnosed with colon or rectum cancers between 2010 and 2016 were 63% and 67%, respectively.2 Individuals diagnosed with localized colorectal cancer (CRC) have an 89% or greater 5-year relative survival rate in comparison to those diagnosed with regional stage CRC (72%) that has spread outside the colon or rectum to nearby areas or lymph nodes.2 CRC screening can prevent CRC by identifying precancerous polyps and allow for removal of these polyps prior to their development into cancer. Regular screening can also find CRC in the localized stage and allow for early treatment while the CRC is small and has not spread beyond the colorectal area.2 Given the overall survival rate and improved survival with early diagnosis and treatment, it is unfortunate that only 68.8% of adults age 50 to 75 years were up to date on their CRC screenings in 2018.1
The Women’s Preventive Services Initiative (WPSI) was created in 2016 to emphasize women’s healthcare needs across a lifespan. These needs include evaluation of health risks, health counseling, preventive screenings, and immunizations using evidence-based guidelines as the foundation to promote health across a woman’s lifetime.3 As part of the WPSI annual preventive care visit, CRC screening is included based on US Preventive Services Task Force (USPSTF) recommendations.4 This article is intended to inform clinicians about CRC risk factors, summarize updated CRC screening guidelines, and discuss current screening tests available.
Colorectal cancer risk factors
Colorectal cancer risk factors can be divided into modifiable and nonmodifiable. Modifiable risk factors include being overweight, lack of physical activity, smoking, alcohol use, and certain types of diets.5,6 Being overweight increases the risk of developing and dying from colorectal cancer.5,6 Maintaining a body mass index in normal range (18.5–24.9) can reduce the risk. Individuals with a sedentary lifestyle are also at increased risk of CRC.5 The American Cancer Society recommends between 150 and 300 minutes weekly of moderate-intensity aerobic activity for adults, along with limiting sedentary behavior.7 Smoking tobacco, especially for a long period of time, increases risk of CRC when compared to nonsmokers.5,6 Moderate to heavy consumption of alcohol has been linked to increased risk of CRC.5,6 The American Cancer Society recommends women consume no more than one alcoholic drink per day.5 Eating a diet high in red meats and processed meats places an individual at a higher risk of developing CRC. Maintaining a diet high in fruits, vegetables, fiber, and whole grains lowers CRC risks.5,7
Some CRC risk factors cannot be changed. These include age, personal health history, family history, race, and ethnicity. Colorectal cancer risk increases with age and is more common in those age 50 years and older.5,6 A personal or family history of adenomatous polyps or prior colorectal cancer increases the risk of CRC. A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease) or type 2 diabetes increases the risk of developing CRC.5,6 An individual’s racial and ethnic background can increase the risk of CRC.5,6 African Americans have the highest CRC incidence and mortality rates in the US, while Jews of Eastern European descent have the highest CRC risks in the world.5,6 Individuals with inherited syndromes such as Lynch syndrome and familial adenomatous polyposis are at higher risk of developing CRC.5,6 Of note, about 5% of individuals diagnosed with CRC have an inherited syndrome.5
Newly released screening recommendations
Recommendations for CRC screening differ slightly among authoritative agencies and can be confusing to decipher. For purposes of this article, guidelines from the American Cancer Society (ACS), the American College of Gastroenterology (ACG), and the USPSTF will be discussed. See Table 1 for a detailed review of CRC screening guidelines.

The ACS provides CRC screening guidelines for average-risk individuals and does not have different parameters for those who are considered at high risk. The ACS recommends regular CRC screenings for all individuals age 45 to 75 years who are healthy with a life expectancy of more than 10 years. For those age 76 to 85, shared decision making should occur for individuals who remain in good health with a life expectancy of more than 10 years. The ACS does not recommend continued CRC screenings for individuals older than age 85.8
In 2021, the ACG updated its 2009 CRC screening guidelines. The updated guidelines include average-risk and high-risk categories with recommendations being labeled as “strong” if supported by moderate-to-high evidence and “conditional” if only supported by low evidence. Unlike the ACS, the ACG provides separate evidence-based guidance for high-risk individuals.8,9 For average-risk individuals, the ACG has strong recommendations for CRC screening for individuals from age 50 to 75 years and conditional recommendations for screening for those age 40 to 49 and 76 to 85 years.9
The USPSTF currently recommends CRC screening for all individuals age 45 to 75 and shared decision making for anyone age 76 to 85 years.6 The updated 2021 guidelines contain two major changes: lowering the age of initial screening from age 50 to 45 and endorsing shared decision making for adults age 76 to 85 years.6,10 The USPSTF has determined a substantial net benefit for CRC screening for individuals age 50 to 75, moderate net benefit for individuals age 45 to 49, and small net benefit for individuals age 76 to 85 years. High-risk individuals include those with a history of CRC, adenomatous polyps, or inflammatory bowel disease; genetic predisposition or family history of CRC; or prior history of radiation to abdomen or pelvic region.6,8,9 Although the USPSTF has identified those at increased risk for CRC, it does not provide additional screening guidelines for these individuals.6
Colorectal cancer screening tests
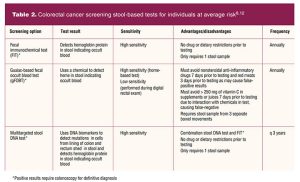
In addition to determining who should be screened based on their age and relative CRC risk, the clinician must decide the best type of screening test for each individual patient.8 Acceptable CRC screening tests can be categorized as stool-based tests or colon and rectum visual exams.8 Stool-based tests include fecal immunochemical test, guaiac-based fecal occult blood test, and stool DNA test. Each test can be performed in the patient’s home through use of a testing kit that includes all necessary collection and testing supplies. Colonoscopy is the most widely used gastrointestinal diagnostic procedure done in the US, but it can result in bleeding and/or perforation.6,9 Clinician and patient shared decision making should occur when deciding which CRC screening test will be ordered. It is important for patients to be aware that positive stool-based tests, flexible sigmoidoscopy, or CT colonography will require a follow-up colonoscopy.6,8,9 See Table 2 for stool-based screening tests and frequency recommendations.
Clinicians should discuss with each patient the importance of checking with their insurance provider about coverage of CRC screening tests and potential out-of-pocket expenses prior to selecting a particular test. The Affordable Care Act requires private insurance and Medicare plans to cover CRC screening tests at no charge to the patient but does not require all services involved with the screening tests (ie, pathology fees, anesthesia charges) to be covered at no costs to the patient.10 Individuals should ask their health insurance provider what costs they are responsible for if further testing is required based on the screening test findings.10 For example, if an individual were to have an abnormal finding on a stool-based test will insurance cover the cost of a colonoscopy?
Implications for older adults
The ACS, ACG, and USPSTF agree that older adults should follow CRC guidelines until the age of 75, participate in shared decision making from age 76 to 85, and discontinue CRC screening at age 86 years.6,8,9 According to the USPSTF, older individuals who have previously received CRC screening with normal results have a small net benefit when continuing screening after their 76th birthday.6 For individuals age 76 to 85 years, shared decision making includes the clinician carefully reviewing the patient’s health history, life expectancy, and prior screening history. Comorbidities and increased risks associated with colonoscopies should be considered when recommending continued CRC screening in this population.6,9 Flexible sigmoidoscopy and colonoscopy require anesthesia, a known risk factor for older adults, and both procedures can result in bleeding and/or perforation. Although the clinician could recommend an alternative, less invasive screening test, positive results will require a colonoscopy for definitive diagnosis.6
Case scenarios
Case scenario 1
Janet is age 51. She lives in a rural community, earning minimum wage as a clerk at the local convenience store. Her husband is a long-haul truck driver. Janet reports that they struggle to meet their household expenses and she is concerned about taking time off to travel to a facility that does colonoscopies and any out-of-pocket expenses that her health insurance does not cover. Janet has never been screened for CRC and denies any family history of CRC or adenomatous polyps. She agrees to a fecal immunochemical test, and the results are positive. How should the clinician respond?
Scenario 1 recommendations
All the discussed CRC screening guidelines recommend a colonoscopy for positive stool-based tests. The clinician should provide the necessary education to help Janet understand the importance of obtaining a follow-up colonoscopy to rule out CRC or an adenomatous polyp. Janet should also receive information about the importance of early cancer detection and treatment. The clinician or office staff can assist Janet in locating a specialist who will accept a payment plan should her insurance not cover all expenses and assist with any transportation needs.
Case scenario 2
Marie is age 32. She is at the clinic today for her annual gynecologic evaluation. When reviewing her health history, the clinician notes that Marie’s older sister was diagnosed with adenomatous polyps at age 43 and her mother was diagnosed with CRC at age 45. Marie asks if she should be concerned about CRC risk. How should the clinician respond?
Scenario 2 recommendations
The clinician should listen emphatically to Marie’s concerns and acknowledge her increased risk for CRC. According to the ACG, Marie should have a screening colonoscopy within the next year, followed by repeat colonoscopies every 5 years.
Case scenario 3
Ruth is age 82. She has mild osteopenia, hypertension well controlled with medication, and a hiatal hernia. She has called your clinic asking if she should be screened for CRC. Her lifelong friend has been diagnosed with stage 4 colon cancer. Ruth admits that even though she has had regular mammograms she has never given much thought to other cancer screenings.
Scenario 3 recommendations
The clinician should engage Ruth in shared decision making by informing her of the risks and benefits of CRC screening. Ruth appears to be in good health with a life expectancy of 10 or more years and so satisfies the criteria for CRC screening. If the patient chooses this after discussion of benefits and risks related to her age, the preferred screening test would be a stool-based test, although a colonoscopy would also be reasonable if the patient chooses this after discussion of benefits and risks related to her age.
Summary of changes from previous guidelines
These are the primary changes from prior screening guidelines:
- Recommend CRC screening starting at age 45 instead of age 50 years in all adults regardless of risk level.6,11
- Recommend continued CRC screening for those age 76 to 85 years within the context of shared decision making based on the individual’s personal and family history.6,10
- Discontinue CRC screening at age 86 years.6,11
Conclusion
Over the years, evidence has continually shown colorectal cancer risk increases with age. More recent studies revealed prevalence of CRC in those age 40 years and older has increased.6 The 2021 colorectal cancer screening guidelines not only account for the younger age of CRC incidence but also offer multiple screening options to remove barriers to screening adherence.6,9 Given the improved survival rate for colorectal cancer with early detection and treatment, recommending CRC screening in keeping with current evidence-based guidelines is an important component of preventive healthcare. The clinician has an important role to educate patients concerning CRC risk factors and risk reduction. Shared decision making can guide the choice of screening test.
Kala K. Blakely is Assistant Professor and Natalie R. Baker is Associate Professor at the University of Alabama at Birmingham School of Nursing. The authors have no actual or potential conflicts of interest in relation to the contents of this article.
References:
- Centers for Disease Control and Prevention. Colorectal (colon) cancer: Colorectal cancer statistics. June 8, 2021.
- American Cancer Society. Survival rates for colorectal cancer. January 29, 2021.
- Women’s Preventive Services Initiative. Recommendations for preventive services for women: final report to the U.S. Department of Health and Human Services, Health Resources & Services Administration. 2016.
- American College of Obstetricians and Gynecologists Foundation. January 2021.
- American Cancer Society. Colorectal cancer risk factors. June 29, 2020.
- US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977.
- Rock CL, Thompson C, Gansler T, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin. 2020;70:245-271.
- American Cancer Society. American Cancer Society guidelines for colorectal cancer screening. November 17, 2020.
- Shaukat A, Kahi CJ, Burke CA, et al. ACG clinical guidelines: colorectal cancer screening 2021. Am J Gastroenterol. 2021;116(3):P458-479.
- American Cancer Society. Insurance coverage for colorectal cancer screening. May 19, 2021.
- US Preventive Services Task Force. Final recommendation statement: colorectal cancer screening. May 18, 2021.
- National Cancer Institute. Screening tests to detect colorectal cancer and polyps. August 2, 2021.

