Pregnant persons have reported low sexual satisfaction, and sexual dysfunction has been measured in up to 91% of pregnant women.1 Similarly, an estimated 35% of women experience sexual dysfunction at 3 months postpartum.2 Optimally, sexual health (SH) discussion moves beyond evaluation for sexually transmitted infections or contraception plans.3 Clinicians, including physicians, nurse practitioners, and nurse-midwives that provide perinatal care may have neither been sufficiently trained nor feel comfortable performing SH assessments.4 Employing an SH assessment tool should assist with this important part of perinatal care.
Currently, no validated perinatal SH assessment tools exist. However, the well-established PLISSIT [Permission, Limited Information, Specific Suggestions, and Intensive Therapy] model is a systematic guide for evaluation of and response to SH concerns demonstrated for use in the perinatal setting.5 It has been studied for counseling use in several populations, including postpartum women. It was found that PLISSIT application improved the sexual quality of life as measured by the Arizona Sexual Experiences Scale.6
Specifically, the model prompts the clinician to begin by giving the patient permission to talk about a sexual subject comfortably in the healthcare setting. Limited information is provided through patient education about any SH concern. Specific suggestions may be provided after a more detailed examination with goal setting and follow-up. A small number of patients may benefit from intensive therapy, which means a referral to a specialist such as a sex counselor or therapist. The PLISSIT model was originally designed for sex therapists but is adaptable to other healthcare settings for assessment, triage, treatment, or referral.7
Clinical Topics: Reproductive and Sexual Health
Hypoactive sexual desire disorder: How do you identify it and treat it?
Project purpose
A chart review of a large suburban women’s clinic revealed that less than 10% of perinatal patients had documentation of SH assessment. The aims of this quality improvement (QI) project were to create a positive shift in attitudes and beliefs of clinicians about perinatal SH assessment facilitating intentionality; and increase perinatal SH assessments by 40% using the PLISSIT model with an electronic medical record (EMR) smart phrase within the chart.
Description of population and setting
The setting for this project was a private obstetrics and gynecology practice at two locations performing approximately 70 deliveries per month. There were 13 clinicians. Among them were six certified nurse midwives, six obstetricians, and a physician’s assistant.
Description of quality improvement project
The project was determined exempt of human subject research by the organization’s Institutional Review Board. All 13 of the clinicians agreed to participate in the project. With consideration that they would need education and support for both the content and incorporation of an SH assessment tool, one educational session was designed by the project innovator to allow for both information sharing as well as discussion of implementation techniques using the PLISSIT model.
Participants completed an anonymous preintervention 22-question Qualtrics administered attitudes and beliefs survey along with a 10-question sexual health knowledge test. The attitudes and beliefs questions were modeled after the Complimentary Alternative Medicine Questionnaire developed by Dr. Desiré Lie.8 The questions reflected beliefs about perinatal SH assessment as well as confidence and competence to perform SH assessment. These elements form the basis for intent.9 Participants read two publications on the model and completed an SH crossword puzzle.1,10 A 45-minute educational session included a brief review of the articles and review of the crossword puzzle key. Four 37- to 72-second trigger videos illustrated clinician–patient interactions, providing examples of when PLISSIT model utilization would be appropriate. Following each video, three discussion questions were explored with participants assessing which PLISSIT elements could be implemented with sample documentation.
The smart phrase (.plissit) was added to the EMR. When the “. plissit” phrase was entered into the EMR, the phrase opened to “The PLISSIT model evaluation strategy was utilized at this visit.”
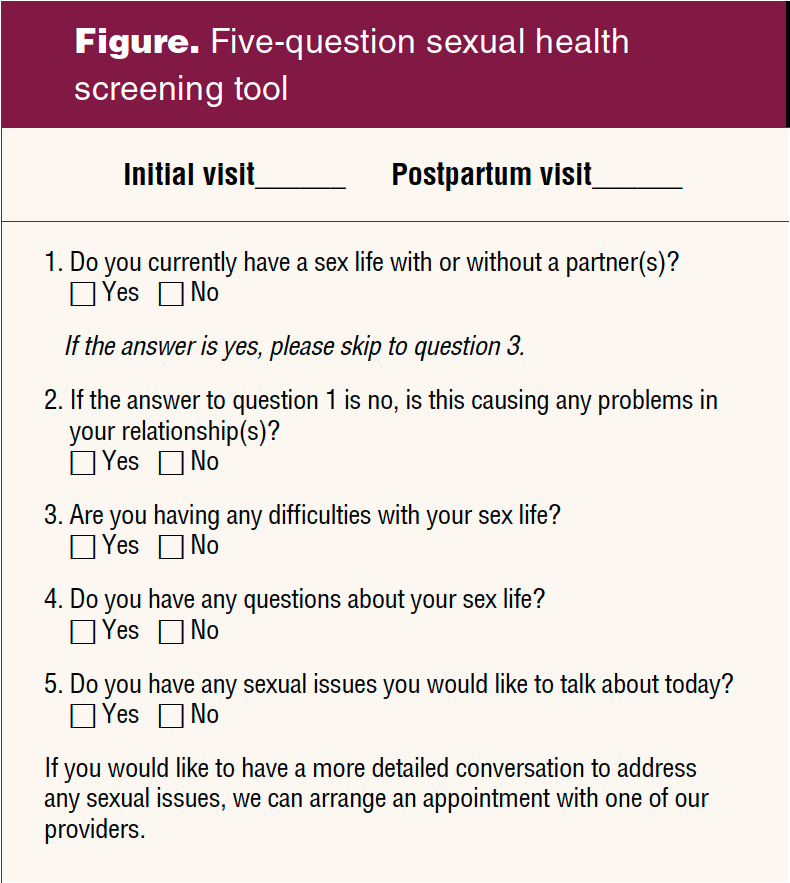
Nursing staff assisted in the project by offering patients a 5-question SH screening tool. Patients gave the completed tool to the providers for review. The SH 5-question screening tool created for the initial prenatal visit and the concluding postpartum visit opened the SH assessment by giving the patient permission to express SH concerns and prompting the provider to respond (Figure). A one-question screening tool was offered at the 20 weeks’ gestation anatomy scan: “Now that you are halfway through your pregnancy, have there been any changes in your sex life, or new sexual issues that you would like to discuss?”
Methods to evaluate outcomes
Charts of pregnant and postpartum patients seen during the 6 weeks’ implementation of the project were reviewed to determine any change in the utilization of SH assessment. Changes in clinician knowledge about SH were measured by comparing results of the SH knowledge scores completed before and immediately after the education session. Changes in clinician beliefs and attitudes were measured by comparing survey scores of the clinicians completed before the education session and at 6 weeks using Wilcoxon signed rank tests. Descriptive analysis of quantitative data was generated using Excel to summarize PLISSIT model implementation and documentation.
Outcomes
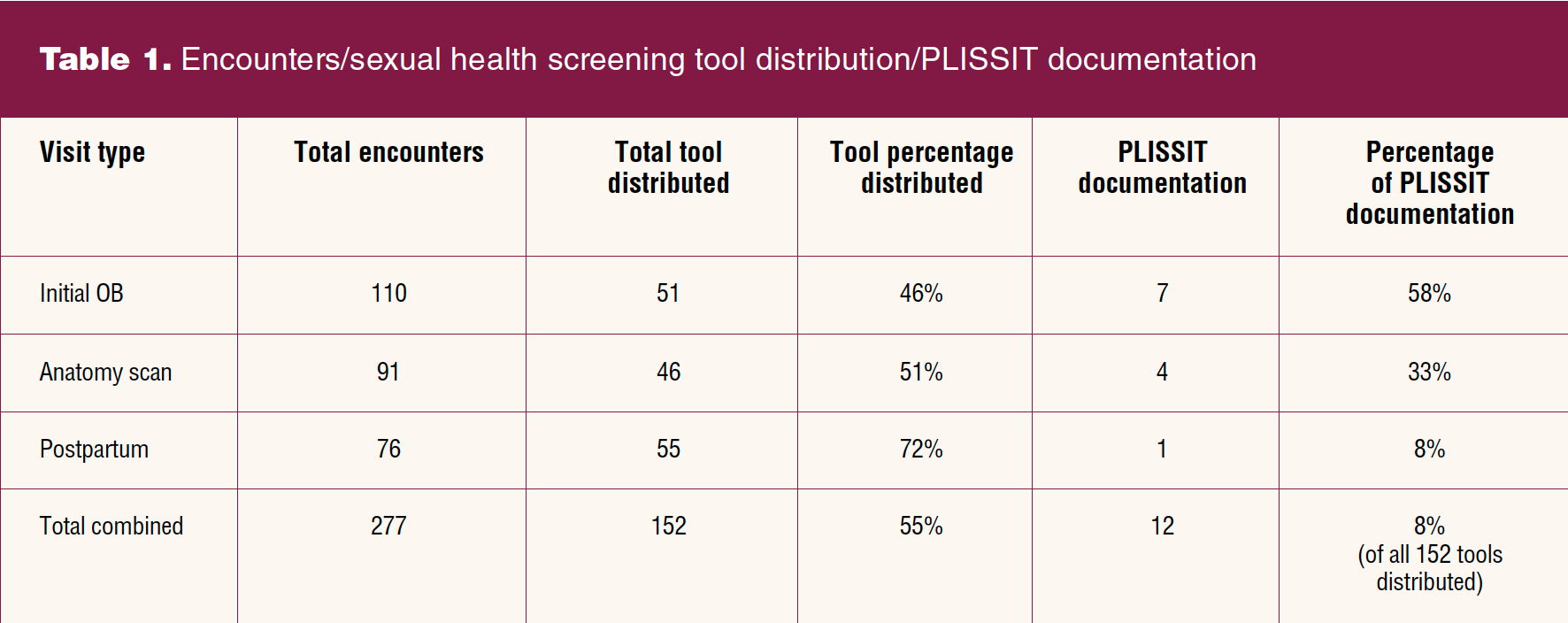
A total of 277 eligible encounters occurred with chart review (Table 1). There were 152 completed tools (55%) showing utilization of SH assessment for a significant increase. Documentation using the .plissit phrase was less evident at 8%. If there were no affirmative responses within the tool, then there was no documentation of SH assessment. The advanced practice clinicians were more likely to incorporate the PLISSIT tool than their physician colleagues, completing PLISSIT documentation on 80% (10/12) of the SH assessments documented in the EMR.
More tools were distributed at the postpartum visits, 72% (76), and less at the initial prenatal visit, 46% (51). Of the 12 PLISSIT-documented charts: seven (58%) were at the initial obstetric visit, four (33%) were at the anatomy scan, and one (8%) was at the postpartum visit.
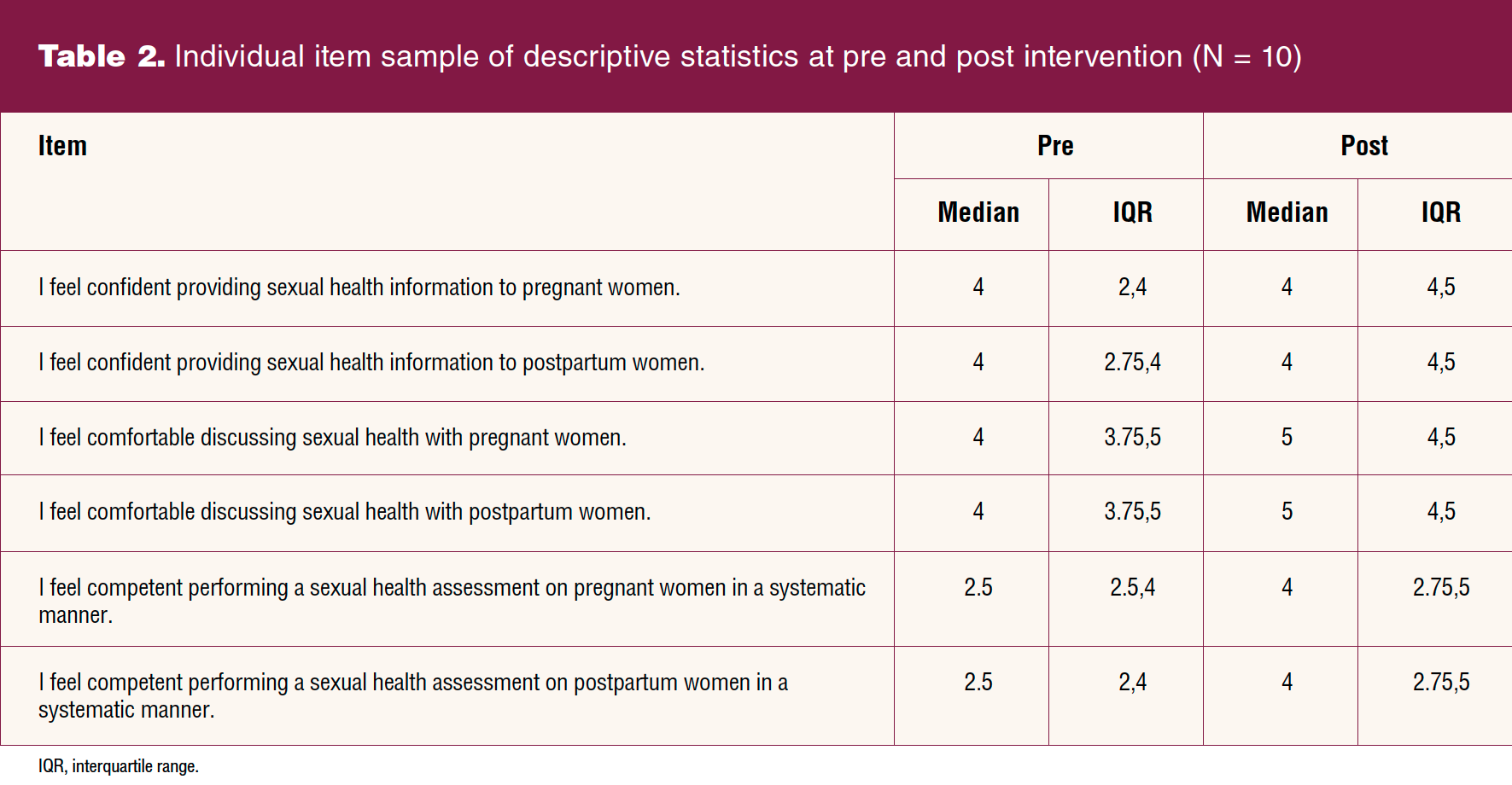
The final sample size, matched for pre and post knowledge surveys and attitudes and belief surveys, was 10 clinicians (three left the practice) (Table 2). Knowledge, well demonstrated in the pretest, improved but not significantly (P = .135). There was an improvement in median attitudes and beliefs of the clinicians from pre (Mdn = 98.50) to post (Mdn = 100.50), but it was not statistically significant (P = .503).
Discussion
Sexual health assessment can be an imposing topic for clinicians partly due to time and partly due to their own discomfort with the topic. Some of the clinicians in this project conveyed concerns that they would not be able to adequately address patients’ sexual concerns. Reviewing the preparation activities, the trigger films, and the promise of readily available consultation when needed gave them a measure of encouragement and willingness to try. A few clinicians reported anxiety specific to two areas: inducing a post-traumatic stress response in patients and/or in the clinician. These concerns were validated by the project innovator. Patient resources for sexual issues were made available to the clinicians. Improved proficiency with the evidence-based PLISSIT model motivated some providers to move forward with SH assessment.
The certified nurse-midwives (CNMs) provided most of the qualifying encounters. Contributing factors could include seeing most of the obstetric patients, having more time to spend with obstetric patients, more affinity, and more cooperation with the innovator who is also a CNM.
For improved efficiency, the SH questions could be embedded within the patient check-in survey in the EMR. This would offer a consistent, sustainable opportunity for SH assessment. Adding PLISSIT to the clinician ROS [review of systems] template with a stop point to answer before chart note completed may help. Providing sex counselor referral lists at stations or on laminated pocket cards may facilitate integration.
Limitations included the small sample size, the short implementation period, and the external impact on education and implementation with the impact of SARS-CoV-2 pandemic.
Conclusion
Sexual health deserves attention as part of women’s total perinatal care. Obstetric clinicians motivated to improve this aspect of care may successfully address this more efficiently using the PLISSIT model. Perinatal sexual health assessments increased in the setting of this project after clinicians attended an education session that included use of the PLISSIT model and with the use of the patient questionnaires and EMR. Continuation of support may be important given the clinicians’ initial expressed concerns. The clinician that wishes to implement QI regarding perinatal sexual assessment may find strategies used in this project helpful.
Cheryl C. Carroll is a DNP graduate at Duke University School of Nursing and on the staff of the Durham Women’s Clinic in Durham, North Carolina. Kathryn J. Trotter is Committee Chairman and Associate Professor; Jacquelyn McMillian-Bohler is a committee member and Assistant Professor; and Julie Thompson is a consultant, all at Duke University School of Nursing in Durham, North Carolina. The authors have no actual or potential conflicts of interest in relation to the contents of this article.
References
1 Afshar Y, Nguyen M, Mei J, Grisales T. Sexual health and function in pregnancy: counseling about sexuality in pregnancy offers an opportunity to allay fears and increase patient satisfaction during a unique period in a woman’s life. Contemp OB/GYN. 2017;62(8):24-30.
2 Dawson SJ, Vaillancourt-Morel M-P, Pierce M, Rosen NO. Biopsychosocial predictors of trajectories of postpartum sexual function in first-time mothers. Health Psychol. 2020;39(8):700-710.
3 American Academy of Pediatrics: Elk Grove Village, Illinois. American College of Obstetricians; Washington, DC. Issuing bodies, 2017.
4 de Oliveira R, Montagna E, Zaia V, et al. The development of cognitive and affective skills through a sexual and reproductive health medical education unit. Sex Med. 2019;7(3):326-336.
5 Nejati B, Kazemi F, Masoumi S, et al. Efficacy of sexual consultation based on PLISSIT model (permission, limited information, specific suggestions, intensive therapy) on sexual function among pregnant women: a randomized control clinical trial. J Isfahan Med School. 2017;35(435):739-748.
6 Abdelhakm E, Elsayed D. Effect of PLISSIT model sexual counseling. Program on sexual quality of life for postpartum women. Am J Nurs Sci. 2018;7(2):63-72.
7 Malakouti M, Golizadeh G, Mirghafourvand M, Farshbaf-Khalili A. The effect of counseling based on ex-PLISSIT model on sexual function and marital satisfaction of postpartum women: a randomized controlled clinical trial. J Educ Health Promot. 2020;9:284.
8 Lie D, Boker J. Development and validation of the CAM Health Belief Questionnaire (CHBQ) and CAM use attitudes amongst medical students. BMC Med Educ. 2004;4(2).
9 Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Addison-Wesley; 1975.
10 Palmisano B. PLISSIT model: introducing sexual health in clinical care. Psychiatry Advisor. January 4, 2017. https://www.psychiatryadvisor.com/home/practice-management/plissit-model-introducing-sexual-health-in-clinical-care/.