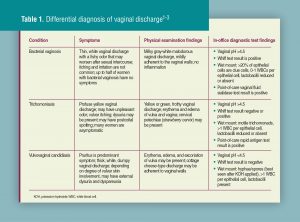
Review of diagnostic tests
The most common in-office tests used to aid in the diagnosis of vaginal infections are a pH test of the vaginal discharge, wet mount microscopic inspection, and a whiff test. Also available are organism-specific point-of-care tests, which have higher sensitivity and equal or higher specificity than those of the wet mount. In some cases, laboratory tests may be indicated for diagnosis.
The pH of vaginal fluid can be determined by placing a strip of pH litmus paper directly on the wall of the vagina or placing discharge from a collection swab on the strip. As an alternative, HCPs can dip the strip into discharge pooled on the upper blade of the speculum. HCPs should avoid using discharge from the posterior vaginal fornix, which might be mixed with cervical secretions and could possibly affect the pH.1-3 The normal pH of the vagina is between 3.8 and 4.5. A vaginal pH less than 4.5 is consistent with physiologic discharge or vulvovaginal candidiasis (VVC). A vaginal pH greater than 4.5 predicts a diagnosis of bacterial vaginosis (BV) or Trichomonas vaginalis infection. When VVC and a concomitant BV or T. vaginalis infection occur, the vaginal pH may be above 4.5. Other factors that can cause an elevated pH include atrophic vaginitis or contamination of the specimen with blood, semen, or urine. A woman who is immediate postpartum, lactating, or menopausal may have an elevated vaginal pH due to reduced systemic estrogen levels. Because vaginal pH testing is not highly specific, the results must be interpreted within the context of a patient’s symptoms, physical exam findings, and wet mount findings.1-4
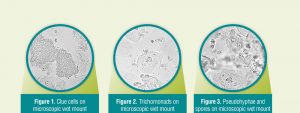
Healthcare providers use a cotton swab to obtain the specimen for a wet mount from the lateral vaginal wall—avoiding contamination with cervical secretions. The wet mount slide can be made by placing a drop of warm 0.9% saline and a drop of the vaginal discharge specimen directly onto it. As an alternative, the swab used to collect the specimen can be placed into a test tube containing less than 1 mL of saline and stirred gently, with a drop of the mixture placed onto a slide. HCPs then place a cover slip over the solution on the slide, followed by immediate examination under a microscope at both low (10x) and high (40x) power. The slide is thoroughly scanned for clue cells and motile trichomonads. Delays of more than 10 minutes in viewing the wet mount significantly reduce the chance of visualizing motile trichomonads required for diagnosis.3
Healthcare providers then place a second sample of the vaginal discharge specimen on a slide and add a drop of 10% potassium hydroxide (KOH) solution. After mixing the sample with the wooden end of the cotton swab or a spatula, HCPs can bring the slide near the nose to perform the whiff test; the presence of a strong amine or fishy odor is considered a positive result. A positive whiff test is consistent with a diagnosis of BV, although it may also be present with T. vaginalis infection. After performing the whiff test, HCPs place a cover slip over the preparation on the slide, followed by examination under the microscope. KOH destroys most of the cells and bacteria, but it does not significantly affect any fungal organisms, thereby making it much easier to visualize pseudohyphae and spores. Pseudohyphae seen on the wet mount confirm the presence of Candida albicans. C. glabrata strains may form spores, but not pseudohyphae, making wet mount detection more difficult.3
Amsel criteria for the diagnosis of BV combine findings from vaginal pH, wet mount microscopy, the whiff test, and characteristics of the vaginal discharge seen on speculum exam. Presence of three of these four criteria provides sufficient evidence for a clinical diagnosis of BV:
• vaginal pH >4.5;
• positive KOH whiff test result;
• clue cells (must constitute ≥20% of vaginal epithelial cells viewed on saline wet mount microscopy); and
• homogeneous, milky-white discharge adherent to vaginal walls.1
FDA-approved point-of-care tests offer the convenience of prompt diagnosis of vaginal infections, along with sensitivity superior to and specificity equal to or better than those of wet mount evaluation. Some tests provide the option for self-collection or clinician collection of vaginal specimens. Point-of-care tests are more expensive than the combination of pH testing, whiff testing, and vaginal microscopy. Therefore, some HCPs may choose to use point-of-care tests only if the traditional in-office tests do not reveal the most likely cause of a patient’s symptoms or a microscope is not available.
The OSOM® Trichomonas Rapid Test detects T. vaginalis antigens; live organisms are not necessary to make the diagnosis.5,6 The OSOM® BVBlue® Test detects elevated activity of vaginal fluid sialidase, an enzyme produced by BV-associated organisms such as Gardnerella vaginalis, Bacteroides species (spp), Prevotella spp, and Mobiluncus spp.7 The vaginal discharge sample for both of these tests can be self collected or clinician collected. Results are available within 10 minutes.
The BD AffirmTM VPIII Microbial Identification Test is a non-amplified molecular test that detects T. vaginalis, various Candida spp, and high concentrations of G. vaginalis.8 This DNA probe-based test requires only one specimen obtained with a sterile swab for all three organisms. To conduct this point-of-care test, HCPs must purchase an automated processor that can run six specimens simultaneously in about 45 minutes. Unless the clinical site does high-volume testing, the expense overrides the convenience.
Laboratory testing technology for both vaginal and cervical infections has shifted from cultures to NAATs that use molecular-based techniques. These tests are designed to amplify nucleic acid sequences (DNA or RNA) that are specific for the organism being detected. NAATs can detect live or nonviable organisms. Several different NAAT-based methods are available, including transcription-mediated amplification (TMA) and polymerase chain reaction (PCR).
The BD MAX™ Vaginal Panel test, an FDA-approved NAAT (PCR), detects the microorganisms responsible for causing BV, trichomoniasis, and VVC. The panel identifies several Candida spp; the most common species, when present, are reported as a group, whereas C. glabrata and C. krusei are reported separately. The panel utilizes a BV algorithm that quantifies the ratio of organisms specific to BV infections to normal vaginal bacteria, including lactobacilli.10 A self- or clinician-collected vaginal swab is used to obtain a specimen for this test.
Several NAAT assays test for Neisseria gonorrhoeae, Chlamydia trachomatis, and T. vaginalis on the same sample.3
Cultures can detect both Candida spp and T. vaginalis. Although a yeast culture is not usually necessary to make a diagnosis of VVC, it may be useful when a wet mount is negative for pseudohyphae or spores but a patient has symptoms and discharge or other signs suggestive of VVC on exam. When a woman has recurrent or persistent symptoms of VVC, a culture can help confirm the diagnosis and identify the species of yeast, if present. However, a culture is of no value if a woman has recently used antifungal treatment.2-4 Culture for T. vaginalis is more sensitive than wet mount but less sensitive and more expensive than NAAT.2,3
Culture for BV is not recommended because no bacteria are specific to BV. Although cultures for G. vaginalis are positive in almost all women with symptomatic BV, the organism is detected in up to 50%-60% of healthy asymptomatic women; therefore, its presence alone is not diagnostic of BV.2,3 An option for clinical settings that lack a microscope or point-of-care testing for BV is to send a vaginal discharge specimen to a laboratory for Gram stain diagnosis.3
A Pap test may identify Candida spp in about 25% of patients with symptomatic VVC. Because cells evaluated on a Pap test are from the cervix and not as likely to be affected by VVC, the Pap test is not sensitive for this purpose.2 If Candida spp are found on a Pap test of an asymptomatic woman, treatment is not required.
For T. vaginalis, the Pap test has a specificity of 96% with liquid-based tests and 92% with slide-based tests.2 However, it has a low sensitivity—similar to that of a wet mount (51%-65%).1,2 The Pap test should not be used as a diagnostic test for T. vaginalis because of the high possibility for false-negative results. In a symptomatic patient, treatment may be considered if the Pap test reveals trichomonas. If trichomonas is found on a Pap test in an asymptomatic patient, an NAAT should be performed to confirm the diagnosis before any treatment is initiated. The Pap test is an unreliable tool for diagnosing BV. If a Pap test suggests a shift in flora in a symptomatic patient, HCPs should perform a vaginal pH, an amine test, and a wet mount. Asymptomatic women do not need further evaluation or treatment.2
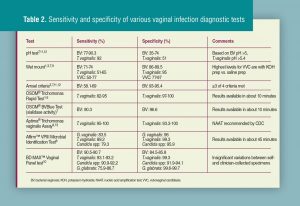
Sensitivity and specificity of diagnostic tests
Sensitivities and specificities for the various vaginal infection diagnostic tests differ. Results must be considered in the context of patient symptoms and physical exam findings. Low sensitivity of a test can result in false-negative results. Low specificity can result in false-positive results. The range of documented sensitivity and specificity for a test may vary depending on the resource and the method of calculation. Table 2 provides the sensitivity and specificity of various vaginal infection diagnostic tests with reference citations.
Implications for clinical practice
When a patient presents with vaginal infection symptoms, making an accurate diagnosis is important so that appropriate treatment can be prescribed. In most cases, the combination of a problem-focused health history and physical exam, along with vaginal pH, wet mount microscopy, and whiff testing, provides sufficient information to pinpoint the cause of a patient’s symptoms. Point-of-care and laboratory tests are available if the diagnosis remains uncertain. When HCPs do not take the time to fully evaluate possible causes of a patient’s symptoms, the result may be persistent symptoms that adversely affect quality of life, repeat visits, overuse of unnecessary antimicrobial medications, and increased healthcare costs.
Beth Kelsey is Assistant Professor at the School of Nursing, Ball State University, Muncie, Indiana; Editor-in-Chief of Women’s Healthcare: A Clinical Journal for NPs; and NPWH Director of Publications, Washington, DC. She states that she does not have a financial interest in or other relationship with any commercial product named in this article.
References
2. Harvard Vanguard Medical Associates and Stewart EG, Bissonnette I, Parks-Forbes D, Margesson LJ. Vulvovaginal disorders: an algorithm for basic adult diagnosis and treatment. 2014. vulvovaginaldisorders.com/
3. National STD Curriculum. Vaginitis. Last updated September 18, 2017. cdn.std.uw.edu/pdf/syndrome-based/vaginal-discharge/core-concept/all.std.uw.edu/pdf/syndrome-based/vaginaldischarge/core-concept/all.
4. Eckert LO. Clinical practice: acute vulvovaginitis. N Engl J Med. 2006;355(12):1244-1252.
6. OSOM® Trichomonas Rapid Test [product insert]. Sekisui Diagnostics LLC. Revised May 2013. sekisuidiagnostics.com/product-documents/osom_trich_181_pi.pdf
7. OSOM® BVBlue® Test [product insert]. Sekisui Diagnostics LLC. Revised May 2016. sekisuidiagnostics.com/product-documents/osom-bvblue_di_3763-11_web.pdf
8. BD AffirmTM VPIII Microbial Identification System [product insert]. Becton, Dickinson and Company. April 2014. legacy.bd.com/ds/technical-Center/inserts/670160JAA(02).pdf
9. Aptima® Trichomonas vaginalis Assay [product insert]. Hologic Inc. January 2019. hologic.com/sites/default/files/2019-04/503684-IFU-PI_005_01_0.pdf
11. Gutman RE, Peipert JF, Weitzen S, Blume J. Evaluation of clinical methods for diagnosing bacterial vaginosis. Obstet Gynecol. 2005;105(3):551-556.
12. Hainer B, Gibson M. Vaginitis: diagnosis and treatment. Am Fam Physician. 2011;83(7):807-815.
13. Prabhu A, Gardella C. Common vaginal and vulvar disorders. Med Clin North Am. 2015;99(3):553-574.

