The author investigated attitudes, beliefs, and knowledge that a group of mothers perceived as compromising or promoting sexual communication with their adolescent daughters. The results of the study are presented and its implications for women’s healthcare providers are discussed.
According to a CDC report, Sexual Activity and Contraceptive Use Among Teenagers in the United States, 2011-2015, 42.4% of never-married female teenagers have had sexual intercourse and 19% of their first sexual encounters have occurred in the absence of birth control.1 Although statistics show that, compared with their counterparts in 1988, slightly fewer adolescents of today are engaging in sex and slightly more are using a form of contraception, these rates are still suboptimal.
 Conversations that parents and their children have about sex have been shown to delay adolescent sexual activity and improve adolescent sexual health-protecting behaviors.2 Parent–adolescent sexual communication (PASC) is the primary mode that parents can use to convey information, values, attitudes, and expectations about sex to their adolescent children.3 Effective PASC is associated with more responsible sexual behavior, including use of condoms and other contraceptives, on the part of adolescents, especially when PASC is initiated prior to their sexual debut.4 PASC has been shown to increase adolescents’ self-esteem, postpone their sexual debut, decrease the number of sexual partners that they have, and reduce rates of both teen pregnancy and sexually transmitted infection.3 Parents can have a major beneficial impact on their children’s healthy sexual development by not only initiating discussions about sex but also increasing the quality and frequency of such discussions as their children reach early adolescence.5
Conversations that parents and their children have about sex have been shown to delay adolescent sexual activity and improve adolescent sexual health-protecting behaviors.2 Parent–adolescent sexual communication (PASC) is the primary mode that parents can use to convey information, values, attitudes, and expectations about sex to their adolescent children.3 Effective PASC is associated with more responsible sexual behavior, including use of condoms and other contraceptives, on the part of adolescents, especially when PASC is initiated prior to their sexual debut.4 PASC has been shown to increase adolescents’ self-esteem, postpone their sexual debut, decrease the number of sexual partners that they have, and reduce rates of both teen pregnancy and sexually transmitted infection.3 Parents can have a major beneficial impact on their children’s healthy sexual development by not only initiating discussions about sex but also increasing the quality and frequency of such discussions as their children reach early adolescence.5
Decades of literature on PASC have provided information on both its facilitators and its barriers. However, much of this research has been done with parents of high-risk adolescents (e.g., those in juvenile detention centers) or with those of minority adolescents. Parents in these studies reported multiple barriers to PASC, including embarrassment and a lack of knowledge, comfort, and ability to communicate effectively with their children.6 A statewide survey of a more demographically diverse group of parents showed that among the 70% of parents reporting difficulty initiating PASC, the most common reason was a concern that their child was not old enough or mature enough for such a discussion.3
Little PASC research has focused on the mother–daughter dyad in particular. Studies investigating the perceptions of mothers regarding sexual communication with their daughters would build on current limited knowledge. The knowledge gained could then inform the development of interventions to promote maternal self-efficacy in initiating mother–daughter sexual communication (MDSC) and continuing to hold such conversations on a regular basis, with the goal of decreasing their daughters’ risky sexual behaviors.
The study
The goal of this study was to contribute to the body of knowledge on MDSC and to develop a deeper understanding of the attitudes, beliefs, and knowledge that mothers perceive as compromising or promoting MDSC. The three aims of this study were to examine the attitudes, beliefs, and content knowledge of mothers of adolescent females; to identify what mothers perceived as major barriers to effective MDSC; and to identify what mothers perceived as major facilitators of effective MDSC.
Methods
Sample
After receiving institutional review board approval, the investigator recruited a convenience sample of mothers residing in one Ohio suburban community who had adolescent daughters aged 11-14 years. Participants were recruited through flyers posted at local venues, via a community networking Facebook page, and by word of mouth. Inclusion criteria were (1) adult female; (2) English speaking; (3) and living with an adolescent daughter aged 11-14 years who has never been pregnant. Informed consent was obtained prior to the interview.
Procedure
One-on-one interviews were conducted to understand MDSC from the perspective of the mother of an adolescent daughter. Open-ended, semi-structured interview ques-tions were derived from the aims. Participants were interviewed one time each for 30-40 minutes. Saturation was reached after 10 interviews. Interviews were audiotaped with a personal digital recorder and transcribed by a hired professional.
Participants completed a demographic survey sheet. Information collected included the ages of mother and daughter, race, ethnicity, occupation, level of education, and marital status. In addition, information about the range of household income and the ages and relationships of other persons in the home where the mother resided was requested.
Analysis
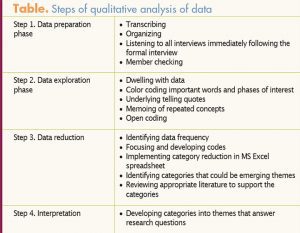
Demographic characteristics were analyzed using central tendencies of the mean, median, and mode. Steps of data analysis and interpretation outlined by Hesse-Biber and Levy were used for the interviews.7 These steps included the data preparation phase, the data exploration phase, the data reduction phase, and the interpretation (Table). The investigator periodically returned to previous steps during this process because coding is an iterative process. In the final steps, themes were developed that represented the most saturated, plausible, supported, and meaningful ideas, concepts, and categories within the data.7
Results
Mean age of the participants was 45.3 years (range, 38-54 years). All identified as non-Hispanic white and were married. Mean age of the daughters discussed in the interviews was 12.7 years (range, 11-14 years). Seventy percent of the mothers worked outside the home. Ninety percent had at least a baccalaureate degree and 60% had a graduate degree. One participant was not a college graduate. Ninety percent reported annual household incomes above $100,000.
ATTITUDES, BELIEFS, AND CONTENT KNOWLEDGE
Mother knows BEST! The most obvious theme that emerged was the belief that it is the mother’s responsibility to be the primary source of sexual health information for her adolescent daughter. Nine of 10 participants held this belief. Participant #1 said her role in MDSC is hugely important. I don’t want it [the information] coming from anyone else. It should be from me, not somebody on the bus.She felt strongly that kids listen to what their parents tell them. She believed it was her responsibility to get them early, and you tell them the facts straight up. Another mother commented, It’s important for the mom to be a source of information, the primary resource for the child, in terms of sex, knowing that it’s a safe place to ask questions, maybe clarify things she has heard. This mother was the first of many to use the term primary resource. Another stated, It’s important for the mom to be a primary resource and start conversations. Participant #4 said, I think the mother is the most important person to talk to the daughter about adolescent sexuality. Participant #5 envisioned herself as the primary source of information, the right information, someone who her child could come to and ask questions and get honest, age-appropriate answers, someone who her daughter can ask about dating or sex or babies or all of that. She saw herself as an educator. Another participant commented on her responsibilities, stating that It’s definitely the mother’s job to bring those conversations to the table with the daughter. I want to make sure she always hears information from me versus students at school, on the bus, or in the classroom. The maternal role in MDSC, as stated by Participant #7, is to educate her on anything that she needs to know. Other participants implied that they were the primary resource when stating that it was their responsibility to raise the topic, prompt conversations, and educate their daughters on sexual health.
 Just ask me!Another common theme was the mothers’ confidence in their content knowledge and ability to answer their daughters’ questions. Participant #1 stated, There is no question I wouldn’t answer; anything is “on the table.” Another participant stated that she didn’t think there were any sexual health questions that would be off limits for her 13-year-old: I would be honest with her no matter what. I think she is at the age that I need to answer her questions. Participant #4 agreed, saying, I would be so excited that she asked me something. I would give her all the answers that I felt were appropriate. If her daughter asked her questions about oral sex, masturbation, sexually transmitted infections, and/or birth control she stated, I want her to get the information from me.She’s going to get the information somehow, so I would rather it come from me. Another participant with a 12-year-old daughter said that she would answer any specific questions about birth control her daughter might ask. Likewise, another participant stated that there wasn’t any question that her 12-year-old might ask that she wouldn’t or couldn’t answer. She commented, If I don’t address her questions, who would she ask? When asked if she would answer any question her daughter might pose about any sexual health topic, Participant #9 took time to think about her answer. She finally replied, I would answer all her questions. I think I’d be uncomfortable talking about oral sex and things like that with her, but I would, obviously, I would answer. Most mothers said that they would answer any questions posed about sexual positions, masturbation, and oral sex, and that they were comfortable answering those types of questions.
Just ask me!Another common theme was the mothers’ confidence in their content knowledge and ability to answer their daughters’ questions. Participant #1 stated, There is no question I wouldn’t answer; anything is “on the table.” Another participant stated that she didn’t think there were any sexual health questions that would be off limits for her 13-year-old: I would be honest with her no matter what. I think she is at the age that I need to answer her questions. Participant #4 agreed, saying, I would be so excited that she asked me something. I would give her all the answers that I felt were appropriate. If her daughter asked her questions about oral sex, masturbation, sexually transmitted infections, and/or birth control she stated, I want her to get the information from me.She’s going to get the information somehow, so I would rather it come from me. Another participant with a 12-year-old daughter said that she would answer any specific questions about birth control her daughter might ask. Likewise, another participant stated that there wasn’t any question that her 12-year-old might ask that she wouldn’t or couldn’t answer. She commented, If I don’t address her questions, who would she ask? When asked if she would answer any question her daughter might pose about any sexual health topic, Participant #9 took time to think about her answer. She finally replied, I would answer all her questions. I think I’d be uncomfortable talking about oral sex and things like that with her, but I would, obviously, I would answer. Most mothers said that they would answer any questions posed about sexual positions, masturbation, and oral sex, and that they were comfortable answering those types of questions.
BARRIERS TO EFFECTIVE MDSC
Let’s wait and see! The first theme that emerged regarding a barrier to MDSC was the daughter’s lack of initiation. Mothers held a universal perception that if their daughter initiated the conversation, that would be a sign that she was ready to discuss the topic. Participant #1 reported an anatomy-focused conversation that sheinitiated with her then 11-year-old daughter about how babies are made. She stated that her daughter did not ask any questions during or after the talk; flash forward 18 months, and the topic still has not been raised again. The mother perceived that her daughter was just so not there. Another participant admitted that she had not yet discussed sex terminology with her 13-year-old because of her daughter’s lack of initiation. Nevertheless, the mother said that she did want to open the dialogue. Another participant reported that conversations occurred only if she initiated them, but that she didn’t want to always be the one doing so because her daughter displayed embarrassment and discomfort. The mother believed that her daughter would eventually initiate the discussion when she was no longer embarrassed or uncomfortable. Other participants supported this approach, with examples such as the following: If she brought it up, I would know that she’s ready for it and She hasn’t really asked a lot about herself. The mothers thought that if their daughters asked questions first, it would be a signal to jumpstart the conversation. Participant #3 couldn’t remember any times when media exposure sparked her daughter to initiate any conversations and therefore she hadn’t done so either. She believed that her 12-year-old might initiate MDSC during her teenage years. This mother also stated she did broach the subject on occasion, but that without her daughter’s participation, the conversations were short and not too informative.
It’s getting uncomfortable. Another perceived barrier that emerged as a theme was the mothers’ perception of their daughters’ discomfort and embarrassment, which usually stopped MDSC in its tracks. More than half the participants gave examples. Participant #6 tried to use sexual health books as a resource for her 12-year-old, who was totally embarrassed and not interested and didn’t even look at them. This mother waited a year to show the resources to her daughter again. Participant #5 validated this perception. When asked if any MDSC occurred prior to the school health talk, she reported, If I would bring up anything about that topic, she would kind of shut down. You could tell it made her uncomfortable. This mother realized that she was missing potential opportunities provided by TV shows and movies to start a discussion about sex with her 14-year-old: I should bring it up at these times, but I don’t because she is so easily embarrassed. Participant #7 allowed her 11-year-old’s comment—Eew, I don’t want to talk about this—to stop a conversation about male and female anatomy. The mother interpreted this comment as a sign that her daughter was not ready. Participant #4 hadn’t yet initiated MDSC because of her concern that her daughter would feel embarrassed and uncomfortable. Other mothers validated this concern. If MDSC was initiated, it often ended quickly because daughters made statements such as Mom, I really don’t want to talk about this and I don’t want to have this conversation right now. Participant #9 noticed that when she told her daughter about the physical mechanism by which babies are made, her daughter listened but had only one comment: I never want to talk about this again. Another participant reported that she tried talking to her fourth-grade daughter following the health talk given at school, but her daughter was really embarrassed and stated that she had no questions and wanted no further discussions.
FACILITATORS OF EFFECTIVE MDSC
It’s coming, It’s coming! Mothers perceived signs of puberty as major facilitators of MDSC. Menses and/or vaginal discharge were the most common occurrences that prompted conversation about sexual health. Participant #1 stated that her daughter came to her because she noticed something in her underwear; her menses had begun. This event provoked questions about menstruation. Another mother said that because her daughter’s period had begun, We talk about it, definitely more frequently and Now that she’s experiencing it and it’s not so mysterious, she’s more comfortable asking questions or coming to me. Her daughter’s menarche led to a discussion about her eggs and how the uterus is preparing itself for a pregnancy. Another participant initiated a conversation because I knew her friends were starting [their periods] so I was able to talk about it. A menses conversation was facilitated for Participant #6 when her daughter expressed concern to her about her discharge-stained underwear. The daughter’s concern paved the way for a conversation about how babies are made. Another mother stated that the start of her 14-year-old’s menses led to questions about not only the menstrual cycle but also puberty in boys versus girls. When her daughter reached menarche, Participant #9 was able to have an in-depth conversation about menstruation. She also introduced the topic of conception because of its relationship to the menstrual cycle. Likewise, when Participant #5 noticed signs of puberty—breast development and pubic hair—in her daughter, she felt more comfortable initiating MDSC.
Follow the academic trail! Scheduled health talks at school served as another important MDSC facilitator for many mothers, some of whom prepared themselves for this talk in advance. Participant #1 stated that she went through all the American Girl health and puberty books right before they had the health chat at school. Another mother held a conversation with her daughter about eggs and sperm prior to the school health talk. She stated, I wanted my daughter to feel as though she knew a lot of what they were talking about.Prior to the school health talk, Participant #8 set the stagefor the information her daughter would learn. Participant #9 also initiated MDSC the night before the talk. She and her daughter had an in-depth discussion about intercourse and conception; she explained that the penis goes into the vagina and then the sperm comes out and connects with the egg. Following the sex chat at school, her daughter asked her all sorts of questions about sex. Many other mothers confirmed that the schoolbased health talks facilitated MDSC. One mother recalled that she and her daughter discussed body hygiene and a girl’s changing body, and about why girls get periods. Participant #4 picked up her daughter after school and specifically asked about the health talk, which prompted a brief conversation in the car about the menstrual cycle. Although another mother expected that her daughter would come home and immediately start a conversation about the sexual health topics discussed at school that day, the daughter held back. However, the mother was pleasantly surprised when, later that evening and again before bedtime, they had conversations about what was discussed at school with regard to puberty and body changes. Participant #7 reported that her daughter did come home and ask a couple of things after the sixth-grade health class. Participant #10 substantiated this theme when she commented, I guess we kind of talked about it [menses] after they spoke about it in school. Participant #3 described a conversation with her daughter regarding sexually transmitted infections as a follow-up to what she learned at school.
Limitations
The primary limitation of this study was the relatively small and homogenous sample—a convenience sample from one suburban community. Another limitation was that participants were interviewed only once, with no follow-up, which potentially limited the volume and depth of data. The data relied on participants’ recall from their own perspective, which injects some recall bias.
IMPLICATIONS FOR PRACTICE AND FURTHER RESEARCH
Advanced practice nurses (APNs) who provide healthcare for female adolescents and women are at the front line when it comes to addressing mothers’ concerns about their daughters’ health, including their sexual health. Promoting MDSC can improve these adolescents’ sexual health and decrease the likelihood of their engaging in risky sexual behaviors. Identifying barriers to MDSC can allow APNs to create and implement interventions that can substitute facilitators for barriers to effective communication. Identifying facilitators can help APNs build upon strategies already working, create resources to strengthen these connections, and show mothers how to capitalize on opportunities to initiate MDSC.
Data from one qualitative study with a focused demographic population is not intended to be generalized to all populations. Nonetheless, this study provides insight through the richness of interviews and developed themes into the attitudes, beliefs, and content knowledge of suburban, middle-class Caucasian mothers of adolescent daughters. Qualitative studies with other demographic populations, conducted via individual interviews or focus groups, would provide a broader perspective and help identify nuances within various populations regarding MDSC. The data gathered from analyzing mothers’ perceptions on MDSC in this study and similar studies with other populations could be used to develop diagnostic tools to identify individual mothers’ strengths and weaknesses with regard to MDSC. This information could be used by APNs to implement interventions that would strengthen mothers’ self-efficacy when encountering perceived barriers and build upon facilitators.
APN-developed interventions could potentially be school or community based, as well as used by individual clinicians in primary care. A partnership among parents, schools, and communities would produce the best outcomes for adolescents’ sexual health. An interdisciplinary approach among pediatric, primary care, women’s health, and mental health providers could also create sustainable interventions to help foster MDSC.
Randee L. Masciola is Assistant Professor at The Ohio State University in Columbus, Ohio, and an actively practicing women’s health nurse practitioner. The author states that she does not have a financial interest in or other relationship with any commercial product named in this article.
References
- Abma JC, Martinez GM. Sexual Activity and Contraceptive Use Among Teenagers in the United States, 2011-2015. National Health Statistics Reports. No. 104. May 22, 2017.
- Askelson NM, Campo S, Smith S. Mother-daughter communication about sex: the influence of authoritative parenting style. Health Commun. 2012;27(5):439-448.
- Jerman P, Constantine NA. Demographic and psychological predictors of parent-adolescent communication about sex: a representative statewide analysis. J Youth Adolesc. 2010;39(10):1164-1174.
- Khurana A, Cooksey EC. Examining the effect of maternal sexual communication and adolescents’ perceptions of maternal disapproval on adolescent risky sexual involvement. J Adolesc Health. 2012;51(6):557-565.
- Martino SC, Elliott MN, Corona R, et al. Beyond the “big talk”: the roles of breadth and repetition in parent-adolescent communication about sexual topics. J Am Acad Pediatr. 2008;121(3):612-618.
- Miller KS, Fasula AM, Dittus P, et al. Barriers and facilitators to maternal communication and preadolescents about age relevant sexual topics. AIDS Behav. 2007;13(2):365-374.
- Hesse-Biber SN, Leavy PL. The Practice of Qualitative Research. Thousand Oaks, CA: Sage Publications; 2006

