This article provides information and care guidelines for healthcare providers who encounter pregnant women who have experienced type 3 female genital cutting (FGC), also known as infibulation. Care needs include counseling regarding risks during pregnancy and birth related to infibulation and sensitivity to the woman’s response to such care as well as her experience and needs related to FGC.
Even though the World Health Organization (WHO), the United Nations Children’s Fund (UNICEF), and the United Nations Population Fund have campaigned since 1997 to eliminate female genital mutilation (FGM), women in a number of areas of the world are still experiencing the practice. It is estimated that 200 million women and girls have experienced FGM.1 Other terminology for the practice includes female genital cutting (FGC) and female circumcision (FC). The term FGM has been replaced by some with either FGC or FC because of the stigma associated with the word mutilation.2–4 UNICEF and the WHO continue to use the term FGM in their ongoing efforts to eliminate the practice, while adding cutting as a hyphenated ending to the term (FGM-cutting).1
The WHO’s advocacy has had impact in some countries, with one example being Kenya, in which the incidence of FGC has decreased over the years.1 The practice also has been declared illegal in a number of countries, but continues despite illegality.5 Advocacy measures to eliminate FGC have been most successful when the local population is convinced to ban the practice and leads the change.2,6 Nevertheless, to this day FGC is performed in over 30 countries. The practice is most often associated with several sub-Saharan African countries but also occurs in Egypt, Iraqi Kurdistan, Yemen, and Indonesia.1 FGC is the cultural norm in these communities, and not being cut has negative consequences. One reason given for proceeding with FGC is that it is required by religion. However, the practice is not advised by any religion and in fact predates Christianity.4,5,7 Other reasons purported for FGC include protecting chastity, preserving ethnic identity, providing aesthetics/beauty and hygiene, and enhancing fertility.5–7 The procedure is done as early as infancy, usually by age 15, and traditionally by lay persons without even local anesthesia, but it has become medicalized in some countries.8–11 FGC is considered a transition to adulthood in some cultures.5
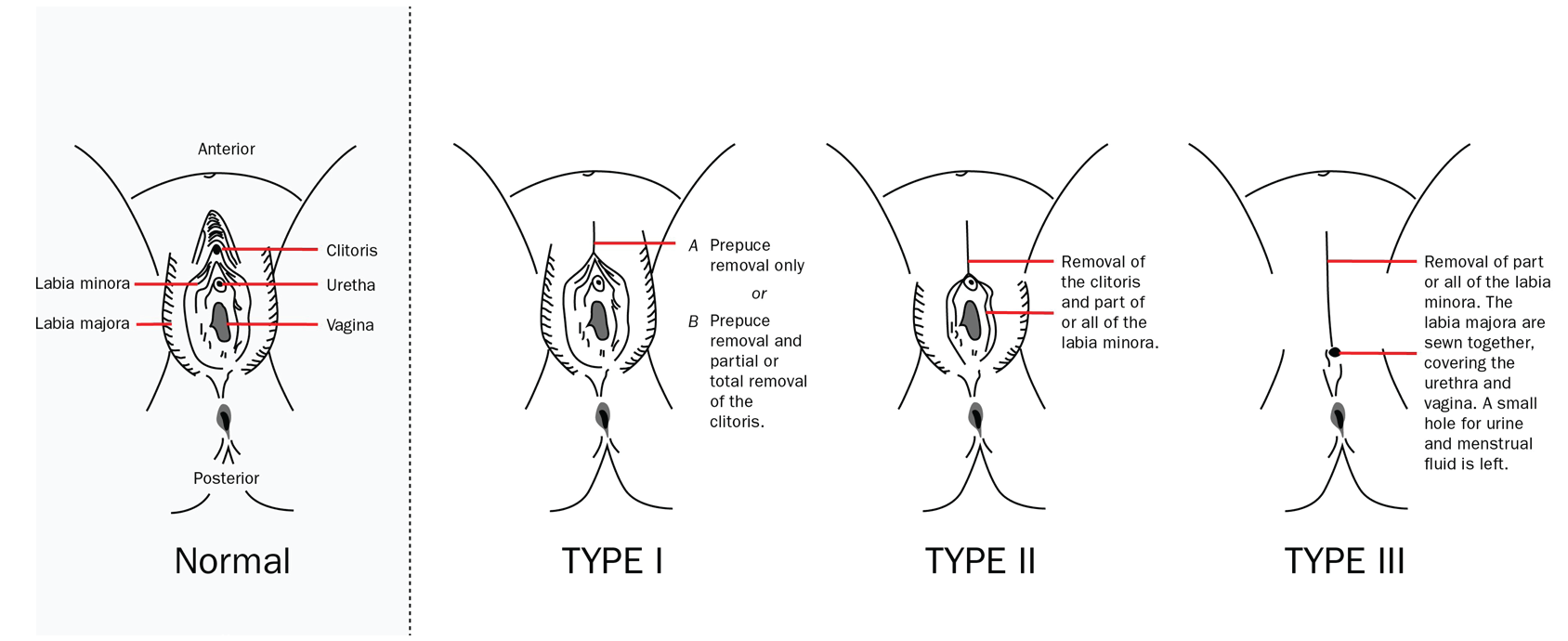
The WHO describes four types of FGC. Type 1 FGC involves partial to total removal of the clitoris and/or prepuce.12 Type 2 involves removal of the labia minora and partial or total removal of the clitoris. Type 3 or infibulation involves removal of the labia minora and all or part of the clitoris with anastomosis of the labial minora (type 3a) and/or labia majora (type 3b), with both types leaving an opening for passage of urine and menstrual flow.12 The opening left with infibulation varies in size and may be as small in diameter as a pencil. Type 4 FGC varies from a pinprick of the clitoris to cauterization of the clitoris or other similar action. Type 3 presents the most challenge for care in the prenatal and perinatal setting.13 Types 1, 2, and 4 present less significant risks during the birth process and challenges for provision of prenatal and perinatal care, even though types 1 and 2 are also associated with increased risk for postpartum hemorrhage and caesarean section.12 See the Figure for a diagram of types 1 to 3 of FGC.
FGC, performed by either medical providers or community laypersons, has been illegal by federal law in the United States for those younger than age 18 years (minors) since 1996. The law has been updated twice.14–16 An update in 2017 made it illegal to transport a minor out of the US to have the procedure, often referred to as vacation cutting.15 The 2021 update clearly describes all types of FGC as illegal and also make it illegal for parents or guardians to consent to such procedure for a minor or take a minor, through either interstate or foreign travel, to an area to have FGC performed. The penalty for performing FGC has increased from a 5- to a 10-year sentence.16 Furthermore, the American College of Obstetricians and Gynecologists (ACOG) condemns FGC at any age as well as identifies any form of female genital cosmetic surgery as generally unnecessary.17,18 Forty states also have passed legislation prohibiting FGC.19 Unfortunately, the practice still occurs in some communities in the US despite these laws and condemnation by professional organizations. Also, dispersion across the globe of individuals who have experienced FGC is growing. Emigration from countries in which FGC is performed is increasing because of internal conflicts and decreasing resources as a consequence of climate change. Many of these migrants have experienced difficult and distressful healthcare encounters with Western providers.20,21 Women’s healthcare providers need to be familiar with FGC, its associated complications, care recommendations to reduce the risks of complications, and the need for a trauma-informed care (TIC) approach to be able to provide quality and respectful care for women who have been cut.13 This article provides an overview about care for women with type 3 FGC during pregnancy and birth.*
Long-term physical and psychological impacts of FGC
Long-term physical impacts include an increased risk for urinary tract infection (UTI), menstrual difficulties, painful intercourse, pelvic inflammatory disease, vaginal odor, scarring that blocks the introitus, and infertility in those who have been infibulated (type 3 FGC).11,13 The flap of tissue covering the urethral meatus is considered the mechanism for the increased risk for UTI and often makes urethral catheterization difficult or impossible. Fusion of the scar tissue to the urethral meatus also can occur, further making ability to catheterize difficult.22,23 Dyspareunia and impaired sexual response are common.4,23,24 Penis in the vagina intercourse may not be possible. Pregnancy in woman for whom vaginal penetration is impossible occurs due to the ability of sperm to swim up the vaginal canal.25
Psychological impacts of FGC include increased incidence of anxiety/depression, nightmares, and neuroses/psychoses that may be worsened in pregnancy. There often also is fear that a healthcare provider might not be familiar with how to manage FGC in pregnancy and psychological distress because of that fear.21 Pregnancy, birth, and the accompanying vaginal examinations make women who have experienced FGC at risk to experience a flashback response to the traumatic event when FGC occurred. That is, the woman may have a post-traumatic stress disorder (PTSD)-like response.4,20,21,26 Assessment for and attention to both physical complications and psychological conditions in women who have experienced FGC are important.
Prenatal care recommendations
Making an appointment to see a healthcare provider for prenatal care can be a difficult decision for a woman who has experienced FGC due to fear that she may be judged for having had the procedure done.3,4,13 So, it is important for the provider to identify and confront their own biases about FGC and any biases in general prior to providing care for those with FGC. Confronting these biases can decrease risk for implicit bias impacting behavior toward the woman.13,27 Use of a TIC approach is also vital to promote a sense of physical and psychological safety for those with FGC.18,28 Using TIC principles of being sensitive to a woman’s life experiences and their impact, using trauma-sensitive language, educating about care, and empowering the woman in regard to care decisions are important practices to adopt for care of women with FGC.28 When obtaining the health history, if the woman indicates she has had FGC, diagrams of uncut external female genitalia and types of FGC can be helpful to explore which type of FGC was performed prior to the physical exam.8 Asking which diagram most closely resembles her genital area is a way to have further discussion about FGC and reassure the woman that you are aware of the practice.
Many women who have experienced FGC come from a culture in which disrobing for a physical examination is not considered acceptable and a female healthcare provider may be preferred.29 A policy on how to meet cultural preferences would be helpful to establish for the clinic and/or hospital practice, especially when there is a known community of individuals who might have experienced FGC. The woman’s privacy should be ensured during the examination, and adaptations should be made to work around clothing. Other providers should not be called into the exam room to view the infibulated genitalia. That is, this is not the time to attempt to create a teaching moment about FGC for colleagues, as such behaviors have often caused embarrassment for the woman and show disrespect.13,21
A pelvic examination has the potential to trigger a PTSD-like response, so it should be deferred unless absolutely necessary.4,20 If a pelvic exam is needed, the provider can discuss the procedure sensitively with the woman, obtain consent, and let her know the exam will be stopped immediately if she experiences distress.8 If specimens are needed and the infibulated opening is too small to allow easy insertion of any speculum, the examiner may collect a sample for Pap or human papillomavirus virus testing and/or cultures by using a blind sweep technique of the vaginal vault.11,25
Clarification of any misconceptions, education regarding what to expect during labor and birth, and discussion of options can allay fears that the woman who has experienced infibulation may have. She may be fearful of unnecessary cesarean section related to a healthcare provider lacking familiarity about how to provide care during birth in the presence of type 3 FGC.13,20 Reasons when cesarean section would be indicated and procedures before and during birth that may decrease the risk should be explained.8,11,30
The option of performing a deinfibulation to prepare for birth should be discussed.11,30,31 Studies indicate there may be an associated increased incidence of perineal tears or trauma, episiotomy, postpartum hemorrhage, and longer postpartum stays for those not deinfibulated antenatally.22,30,32 Obstructed labor and resulting fistulas are also a risk for those who have not been deinfibulated.11,26 Deinfibulation allows for easier vaginal exams to monitor labor, application of scalp electrodes if needed, and other procedures that may be indicated in labor.13
Some experts maintain that the best timing for the deinfibulation procedure is in the second trimester to allow for healing of the tissue prior to the onset of labor.13,23,31 Partial deinfibulation (opening to urethral meatus) or full deinfibulation (opening to clitoris) can be offered options.33 Some recommend deinfibulation be performed at the time of giving birth, and yet others have found no impact in relation to the timing of deinfibulation on risk for cesarean section.33,34
Deinfibulation is a minor surgical procedure used to re-open the vaginal introitus. If it is performed in the second trimester, either regional or general anesthesia is recommended for the procedure, and if it is performed during labor, epidural anesthesia is recommended. Providers performing deinfibulation should have training and experience. Referral to a provider with expertise may be needed. The infibulated tissue is opened using an episiotomy scissors, being careful not to injure the urethral meatus, and the opened labial tissue is separately sutured with subcuticular stitches using absorbable suture materials.11,13,31 Education about increased urine stream after deinfibulation needs to be provided. Postprocedure sitz baths and pain medication are appropriate to aid the healing process.13 Informing the woman and her partner about risks and benefits in regard to timing of deinfibulation and allowing choice about the timing are important in establishing a trusting relationship.21
Discussion about reinfibulation and stitching back together the deinfibulated tissue should also occur as part of prenatal counseling. Involving the woman’s partner in the decision about reinfibulation is recommended, as culturally there may be reliance on partner support and the woman may think reinfibulation is desired when in fact her partner may not want it done.2,33 Therefore, shared decision making is important.35 Although reinfibulation is not recommended by the WHO or the International Federation of Gynecology and Obstetrics and is illegal in the United Kingdom as well as some other countries, it is legal according to federal law in the US to be performed for medical purposes following birth.16,22,33 Informed consent regarding risks and benefits needs to be obtained, and providers should have expertise regarding the procedure.2,29,33 However, whether reinfibulation can be performed may vary according to state law, as some states ban FGC for women of any age.17 Providers must be aware of the law in their practice state.17,18
Discussion about risks and benefits of episiotomy also should occur prior to labor and birth. An episiotomy may be indicated in addition to deinfibulation to decrease risk for anal sphincter tears and postpartum hemorrhage.36 Midline episiotomies are more commonly done in the US. The woman might expect a mediolateral episiotomy, as that practice is more common in other countries, and so discussion about faster healing with a midline episiotomy should be considered.11
Additionally, there may be an increased risk of preeclampsia/eclampsia. Women with type 3 FGC were found to have more than 2 times the risk for preeclampsia (odds ratio, 2.5; 95% confidence interval, 1.4–4.6) in a recent study of women in Mali. An inflammatory response to UTI and/or bacterial vaginosis impacting placentation has been hypothesized to be the mechanism for increased risk of preeclampsia/eclampsia in those who have had type 3 FGC.37
Intrapartum care recommendations
The birth process presents other risks for women with FGC. Use of stirrups and/or assisting with pulling back legs when pushing in the second stage of labor may cause a flashback response to the episode of being restrained when FGC occurred and cause additional stress for the woman.21 Care providers need to be cognizant of this risk and adapt techniques as needed to reduce it.
Deinfibulation risks and benefits and reinfibulation risks need to be reviewed or initiated if not completed prenatally. Reinfibulation, if legal to perform in the practice state, may occur immediately after birth and is performed using an absorbable suture in a process and timing similar to repair of any episiotomy, vulvar, or perineal tears that may occur during the birth process.13
Postpartum care recommendations
Increased risks after giving birth include postpartum hemorrhage, postpartum depression, and unsutured labial remnants deinfibulated or lacerated during birth healing together (re-fusing of tissue). The increased risk for postpartum hemorrhage is most closely related to prolonged labor in those for whom deinfibulation is not performed.36 There may be slower healing of any repair related to scar tissue from the previous FGC.23 The scar tissue also increases risk for dehiscence of episiotomies or other repaired tissue as well as wound infections.13
Women who have been deinfibulated and not reinfibulated should be offered counseling as their new appearance may be stressful.8,33 The woman also may be upset and embarrassed by the ease of urination and the force accompanying the flow of urine, as previously they experienced only a small trickle during urination because of the blockage from infibulation.33 Education prior to deinfibulation about what changes to expect in genitalia appearance and in urination, menstruation, and sexual intercourse are important as anticipatory guidance and should be addressed in follow-up visits.
Conclusion
Infibulation is associated with many risks during pregnancy and birth. Women’s healthcare providers need to be aware of these risks and develop competence for care of those who have experienced type 3 FGC as well as understand that type 1 and 2 also may be associated with increased risk for postpartum hemorrhage and cesarean section. Understanding how to provide informed, sensitive, nonjudgmental, culturally safe care for women with FGC is a crucial component of delivery of quality care by women’s healthcare providers.
Diane Schadewald is Clinical Professor at the College of Nursing, University of Wisconsin–Milwaukee. The author has no actual or potential conflicts of interest in relation to the contents of this article.
References
1 United Nations Children’s Fund. Female genital mutilation. 2021. https://data.unicef.org/topic/child-protection/female-genital-mutilation/.
2 Braddy CM, Files JA. Female genital mutilation: cultural awareness and clinical considerations. J Midwifery Womens Health. 2007;52(2):158-163.
3 Jacobson D, Grace D, Boddy J, Einstein G. Emotional health work of women with female genital cutting prior to reproductive health care encounters. Qual Health Res. 2022;32(1):108-120.
4 O’Neill S, Pallitto C. The consequences of female genital mutilation on psycho-social well-being: a systematic review of qualitative research. Qual Health Res. 2021;31(9):1738-1750.
5 Koski A, Heymann J. Changes in support for the continuation of female genital mutilation/cutting and religious views on the practice in 19 countries. Glob Public Health. 2019;14(5):696-708.
6 Van Bavel H, Coene G, Leye E. Changing practices and shifting meanings of female genital cutting among the Maasai of Arusha and Manyara regions of Tanzania. Cult Health Sex. 2017;19(12):1344-1359.
7 Jacoby SD, Smith A. Increasing certified nurse-midwives’ confidence in managing the obstetric care of women with female genital mutilation/cutting. J Midwifery Womens Health. 2013;58(4):451-456.
8 von Rège I, Campion D. Female genital mutilation: implications for clinical practice. Br J Nurs. 2017;26(18):S22-S27.
9 El-Gibaly O, Aziz M, Hussein SA. Health care providers’ and mothers’ perceptions about the medicalization of female genital mutilation or cutting in Egypt: a cross-sectional qualitative study. BMC Int Health Human Rights. 2019;19:26:1-12.
10 Ahmed W, Mochache V, Stein K, et al. A hybrid, effectiveness-implementation research study protocol targeting antenatal care providers to provide female genital mutilation prevention and care services in Guinea, Kenya and Somalia. BMC Health Serv Res. 2021;21(1):109.
11 World Health Organization. Care of Girls and Women Living with Female Genital Mutilation: A Clinical Handbook. World Health Organization; 2018.
12 World Health Organization. Eliminating female genital mutilation: An interagency statement UNAIDS, UNDP, UNECA, UNFPA, UNHCHR< HNHRC, UNICEP, UNIFEM, WHO. World Health Organization, 2008.
13 Nour NM. Female genital cutting: clinical and cultural guidelines. Obstet Gynecol Surv. 2004;59(4):272-279.
14 18 U.S. Code §116. Federal Prohibition of Female Genital Mutilation Act of 1995. https://www.congress.gov/104/bills/hr941/BILLS-104hr941ih.pdf.
15 18 U.S. Code §116 https://www.govinfo.gov/content/pkg/USCODE-2017-title18/pdf/USCODE-2017-title18-partI-chap7-sec116.pdf.
16 18 U.S. Code §116. Strengthening the Opposition to Female Genital Mutilation Act of 2020. https://www.congress.gov/116/plaws/publ309/PLAW-116publ309.pdf.
17 American College of Obstetricians and Gynecologists. Female genital mutilation. Statement of Policy. 2019.
18 American College of Obstetricians and Gynecologists. Elective female genital cosmetic surgery. Committee opinion 795. Obstet Gynecol. 2020;135(1):e36-e42.
19 Parker A, Zarubin G. Why we hesitate to protect girls from FGM in the United States. Executive summary. AHA Foundation. 2021. https://www.theahafoundation.org/wp-content/uploads/2018/05/Why-we-hesitate-to-protect-girls-from-FGM-in-the-United-States.pdf.
20 Scamill M, Ghumman A. The experience of maternity care for migrant women living with female genital mutilation: a qualitative synthesis. Birth. 2019;46(1):15-23.
21 Wood R, Richens Y, Lavender T. The experiences and psychological outcomes for pregnant women who have had FGM: a systematic review. Sex Reprod Healthc. 2021;29:100639.
22 Albert J, Bailey E, Duaso M. Does the timing of deinfibulation for women with type 3 female genital mutilation affect labour outcomes? Br J Midwifery. 2015;23(6):430-437.
23 Daley A. Female genital mutilation: consequences for midwifery. Br J Midwifery. 2004;12(5):292-298.
24 Esho T, Kimani S, Nyamongo I, et al. The ‘heat’ goes away: sexual disorder of married women with female genital mutilation/cutting in Kenya. Reprod Health. 2017;14(164).
25 Mistry H, Jha S. Pregnancy with a pinhole introitus: a report of two cases and a review of the literature. Eur J Contracept Reprod Health Care. 2015;20(6):490-494.
26 Mwanri L, Gatwiri GJ. Injured bodies, damage lives: experiences and narratives of Kenyan women with obstetric fistula and female genital mutilation/cutting. Reprod Health. 2017;14(1):38.
27 Mkandawire-Valhmu L. Cultural Safety, Healthcare and Vulnerable Populations: A Critical Theoretical Perspective. Routledge, Taylor & Francis Group; 2018.
28 Quaile HC, Benyounes-Ulrich J. Trauma-informed care. Part 1: the road to its operationalization. Womens Healthcare. 2021;9(3):32-36.
29 Hess RF, Weinland J, Saalinger NM. Knowledge of female genital cutting and experience with women who are circumcised: a survey of nurse-midwives in the United States. J Midwifery Womens Health. 2010;55(1):46-54.
30 Okusanya BO, Oduwole O, Nwachuku N, Meremikwu MM. Deinfibulation for preventing or treating complications in women living with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynaecol Obstet. 2017;136(suppl 1):13-20.
31 Gupta S, Latthe P. Female genital mutilation de-infibulation: antenatal or intrapartum? Obstet Gynaecol Reprod Med. 2017;28(3):92-94.
32 Belihu F, Small R, Davey M. Episiotomy and severe perineal trauma among Eastern African immigrant women giving birth in public maternity care: a population based study in Victoria, Australia. Women Birth. 2017;30(4):282-290.
33 Abdulcadir J, McLaren S, Boulvain M, Irion O. Health education and clinical care of immigrant women with genital mutilation/cutting who request postpartum reinfibulation. Int J Gynaecol Obstet. 2016;135(1):69-72.
34 Taraldsen S, Vangen S, Øian P, Sørbye IK. Female genital mutilation/cutting, timing of deinfibulation, and risk of cesarean section. Acta Obstet Gynecol Scand. 2021;100(4):587-595.
35 Johnsdotter S, Essén B. Deinfibulation contextualized: delicacies of shared decision-making in the clinic. Arch Sex Behav. 2021;50(5):1943-1948.
36 Rodriguez MI, Seuc A, Say L, Hindin MJ. Episiotomy and obstetric outcomes among women living with type 3 female genital mutilation: a secondary analysis. Reprod Health. 2016;13(1):131.
37 Bellizzi S, Say L, Rashidian A, et al. Is female genital mutilation associated with eclampsia? Evidence from a nationally representative survey data. Reprod Health. 2020;17(1):68.
Key words: female genital cutting, infibulation, female circumcision, female genital mutilation, pregnancy, care guidelines, perinatal
Womens Healthcare. 2022;10(5):37-42. doi: 10.51256/WHC102237

