The National Association of Nurse Practitioners in Women’s Health (NPWH) asserts that climate change has a significant effect on health and wellbeing globally. NPWH believes that nursing organizations and the nursing profession have a responsibility to meaningfully contribute to reducing vulnerability to the harmful effects of climate change (adaptation) and reducing or preventing greenhouse gas (GHG) emissions (mitigation) for the protection of the health and wellbeing of individuals, communities, and populations. NPWH recognizes that social and environmental justice are inherently connected to reducing harms to health and wellbeing associated with climate change. NPWH advocates for global and national policies and practices that promote strategies to reduce these harmful health effects within a socially and environmentally just framework.
NPWH acknowledges that gender-based disparities exist in health effects related to climate change. Physiologic and biologic vulnerabilities and socioeconomic and racial/ethnic disparities and discrimination are frequently more pronounced for women.1,2 Women living in low- and middle-income countries are the most susceptible. Even in resource-rich countries such as the United States, however, vulnerabilities and disparities in health effects related to climate change fall disproportionately on women. Healthcare informed by these health risks, vulnerabilities, and disparities is imperative. NPWH champions the essential role and expertise of women’s health nurse practitioners (WHNPs) in providing healthcare for women across the lifespan that includes attention to health risks related to climate change. NPWH commits to strengthening efforts in support of this role, with a particular focus on reducing associated health disparities.
NPWH recognizes a need for extensive research to advance scientific knowledge about health effects related to climate change and adaptation and mitigation strategies. Additionally, more research is needed to understand the associations between gender and health risks related to climate change across the lifespan.
A concerted effort is necessary to reduce the harmful effects from climate change on women in a socially and environmentally just manner. NPWH provides leadership and collaborates with other organizations and agencies to deliver continuing education and resources for WHNPs and other advanced practice registered nurses (APRNs) who provide healthcare for women, develop policies, and support research to sustain this effort.
Background
Climate change refers to the changes in the state of the climate attributed directly or indirectly to human activity that alter the composition of the global atmosphere and that persist over time.3 Climate change is the direct result of the rise in global concentrations of GHGs in the atmosphere. GHGs (eg, carbon dioxide, nitrous oxide, methane) absorb and re-emit heat, acting as insulators that increase the temperature of the earth’s atmosphere referred to as global warming.4 Major sources of these GHGs come from burning fossil fuels (eg, coal, petroleum, natural gas, peat) for energy production and use, transportation, and industry. Agriculture contributes to GHGs through use of fertilizers containing nitrogen, a major source of nitrous oxide, and the production of methane as a byproduct of the digestive processes of livestock.4 The concentrations of GHGs have increased significantly causing a 1.5°F increase in the earth’s average temperature over the past 100 years with projections of continuing increases.4,5 The same sources of GHGs are also responsible for an increase in fine particulate matter pollutants in the air and chemicals trapped in the atmosphere by ground-level ozone.6
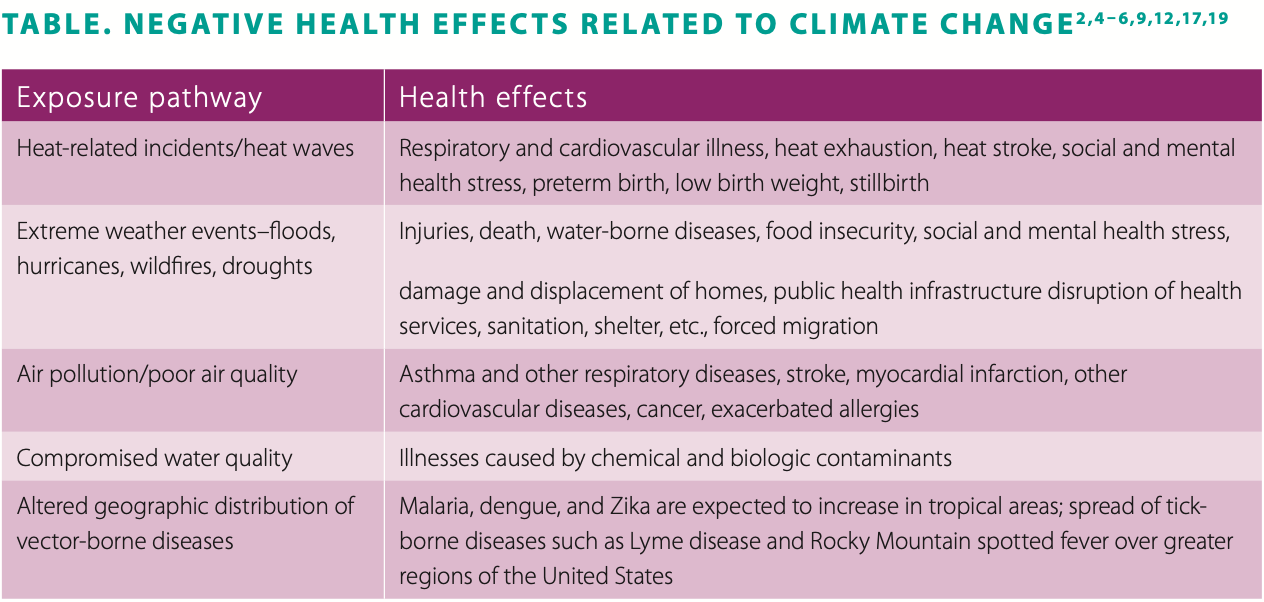
The relationship between climate change and health is complex. The exposure pathways through which health is affected include heat-related incidents, extreme weather events (eg, floods, hurricanes, wildfires, droughts), poor air quality, compromised water quality, food insecurity, and altered geographic distribution of vector-borne diseases. Geographic and socioeconomic factors influence health risks and consequences. The cumulative and interactive effects of climate change adversely affect not only physical health but also mental health.7 Multiple, repeated, and extended contacts with these exposure pathways lead to increased stress levels and decreased resilience for individuals and communities. See Table for examples of negative health effects related to climate change. See Box for select climate change and health terminology.
Vulnerability to the negative effects of climate change is unequally distributed.2,4,9–12 Understanding the nature of these vulnerabilities is crucial to tailoring policies and strategies that recognize ethical and human rights issues. Environmental justice is achieved only by ensuring no individual or community has an unequal share of harmful environmental exposures and all have equal access to adaptive capacity to prepare and plan for, respond to, and recover from adverse climate change events.3,4,12,13 Intergenerational equity is also a component of environmental justice, for which there is an obligation to consider and balance the interests, rights, and well-being of future generations with those of the present generation.14
Around the globe, the most vulnerable populations include pregnant women, fetuses, children, older adults, individuals with chronic health conditions or disabilities, Indigenous peoples, and individuals living in communities that have been socially or economically marginalized.3 The topography, economics, population density, and quality and availability of primary healthcare within any country or region influence susceptibility to and resilience against the effects of climate change.3
Global health organizations, among them, the International Council of Nurses, International Federation of Obstetrics and Gynecology, the United Nations Convention on Climate Change, and the World Health Organization highlight the vulnerability of women to the health-related impacts of climate change.1,3,15,16 In formal statements, all of these organizations affirm that women, especially those living in poverty, are the most at risk for these related adverse health and wellbeing outcomes.1,3,15,16 Maternal health and mental health are two areas in which women have disparate vulnerabilities. These vulnerabilities exist in both resource-rich and resource-challenged countries.
There is emergent evidence and growing concern about a potential relationship between climate change and negative obstetric outcomes. A systematic review of international studies on climate change-related exposures and adverse obstetric outcomes provides evidence of an association between extreme heat exposures and preterm birth, low birth weight, and stillbirth, as well as neonatal heat-related stress.17 Another systematic review of studies across diverse US populations analyzed associations between air pollutants and excessive heat exposure and obstetric outcomes. Nine of 10 studies found a significant association between exposure to heat during pregnancy and preterm birth, low birth weight, and/ or stillbirth.18 Exposure to fine particulate matter pollutants or ozone was associated with preterm birth in 19 of 24 studies and with low birth weight in 25 of 29 studies. This review revealed that women with pre-existing health conditions such as asthma, residence in urban areas with higher levels of air pollution, women of color, and those with long-term high levels of stress were at disproportionate risk for adverse outcomes.18
It is recognized in both systematic reviews that the causes of adverse obstetric outcomes are complex and multifactorial.17,18 Plausible explanations point to alterations in maternal and placental physiology. Heat exposure may contribute to dehydration, altered blood viscosity, and inefficient thermoregulation increasing the risk for preterm labor and birth. Inhalation of toxic fine particulates may trigger systemic and placental inflammation, alter maternal respiratory and cardiovascular function resulting in reduced efficiency of placental function, and cross the placenta resulting in direct toxic effects on the fetus.18 More research is needed to fully understand the mechanism by which these exposures can impact obstetric outcomes so that evidence-based strategies for reducing risks can be implemented at individual and community levels.8
Mental health consequences related to extreme weather events range from minimal stress to clinical disorders that include anxiety, depression, post-traumatic stress disorder (PTSD), and suicidal thoughts.7 Individuals with pre-existing mental health conditions are especially vulnerable to negative post-traumatic reactions after extreme weather events. Disruptions in mental health services and access to medications can further affect health and recovery.6,7 Women have a higher prevalence of PTSD and other mental health disorders after disasters than men and are more prone to greater worry and feelings of vulnerability. Pregnant women have a higher risk of developing postpartum depression after a major disaster in their area.7 Increases in physical, sexual, and intimate partner violence directed toward women are also common after a disaster.2,4
In the US, healthcare providers and public health professionals are increasingly aware of health problems associated with climate change.4 The climate change exposure pathways, types of health problems, and severity vary regionally and locally. Climate change is causing more frequent heat waves. Extreme weather events such as floods, droughts, wildfires, and hurricanes have tripled since the 1960s.4,5 Some communities are in vulnerable locations, some have fewer resources to adapt and protect themselves, and some have suffered social injustices that make them more vulnerable from the beginning. Populations within the US that are most vulnerable are individuals living in poverty, immigrant groups, some communities of color, Indigenous peoples, older adults, individuals with pre-existing health conditions, children, and pregnant women.2,10,19
Some immigrant groups, communities of color, and individuals living in poverty have a higher likelihood of living in risk-prone areas (eg, urban heat islands, isolated rural areas, flood-prone areas), areas with poorly maintained infrastructures, and areas with an increased burden of air pollution. Indigenous peoples who are dependent on their environment for sustenance and those who live in isolated or impoverished communities may be more susceptible to food and water insecurities and degraded infrastructures.2,4,10 Older adults and individuals with chronic physical and mental illnesses and disabilities are at greater health risk during extreme and prolonged periods of heat. Individuals with pre-existing cardiac and respiratory conditions are more susceptible to health impacts triggered by air pollution.2,4,10,19 Physiologic and developmental factors and the usual behaviors and activities of children can increase their exposure to heat-related illnesses, vector-borne and waterborne disease, and respiratory effects from air pollution and allergens.4,10,19 During extreme weather events, many individuals from vulnerable groups may not be able to evacuate and may be cut off from healthcare, medications, clean water and food, electrical power, and shelter. The ability for women to navigate emergency evacuation can be complicated by their role as major caregivers of children, the elderly, and family members with disabilities.1 Subsequent displacement from homes and communities can prolong the interruption in healthcare, which is especially concerning for pregnant and postpartum women and women with young children.
Climate change represents an urgent health challenge that requires engagement, advocacy, and leadership from the nursing profession.9 Nurses must be prepared to provide expertise on behalf of patients, communities, organizations, and policy makers.20 Several professional nursing organizations have formally recognized that climate change and associated health risks are issues that nurses must address. Among them are the Alliance of Nurses for Healthy Environments (ANHE), American Academy of Nursing, American College of Nurse-Midwives, American Nurses Association, Canadian Nurses Association, and International Council of Nurses. These professional nursing organizations call for climate-informed strategies to reduce risks to health, enhance community resilience, and address inequities. 3,21–25
NPWH has partnered with ANHE to lead an effort to address environmental health as a women’s health issue. Through this partnership, representatives from nursing organizations representing women’s, maternal, and child health have come together as the Nursing Collaborative on Environment, Maternal-Child, and Women’s Health. This collaborative is developing an action plan for nursing education, research, practice, and policy regarding the intersection of women’s and maternal-child health and the environment. We must have a collective call to action to address climate change, women’s health, and environmental justice.
NPWH recommendations for women’s health and healthcare
WHNPs and other APRNs who provide healthcare for women have many opportunities to be actively involved in addressing the issue of climate change and women’s health within an environmentally just framework. These opportunities exist within clinical practice, healthcare systems, community advocacy, academia, research, and individual stewardship for the environment. As examples, NPWH recommends that WHNPs and other APRNs who provide healthcare for women:
- Include an environmental assessment as part of maternal health visits and well-woman visits across the lifespan to determine if there are risks or vulnerabilities that need to be addressed.
- Provide education and anticipatory guidance to help patients understand how health conditions are impacted by climate change and what actions they can take to adapt and lessen effects.
- Work with local and state health departments and healthcare facilities to ensure disaster preparedness plans and training are in place for extreme weather events and climate adaptation plans for heat waves.
- Promote public awareness about health impacts of climate change and the health benefits of solutions.
- Advocate for local, national, and global policies regarding climate change that incorporate women’s health concerns as well as those of other vulnerable populations.
- Incorporate content in nursing education curriculum to address the health impacts of climate change, vulnerable populations, environmental justice, and strategies for adaptation, mitigation, and resilience.
- Conduct research that advances scientific knowledge about the associations between gender and health risks related to climate change and effective adaptation and mitigation strategies.
Commit to being good stewards of the environment through professional and personal actions to reduce GHG emissions.
NPWH leadership
NPWH advocates for meaningful contributions by professional nursing organizations and individual nurses to reduce the harmful health effects of climate change on individuals, communities, and populations. As the professional organization for WHNPs and other APRNs who provide women’s healthcare, NPWH commits to concerted strategies to address gender-based vulnerabilities and disparities in relation to the harmful effects of climate change. NPWH will provide leadership to ensure:
- Continuing education (CE) programs and resources are available for WHNPs and other APRNs who provide healthcare for women to increase knowledge about health risks associated with climate change and to be able to use adaptation and mitigation strategies to address these risks at individual, community, and population- based levels.
- CE programs and other evidence-based resources are available to assist WHNP program faculty to develop curricula that include health impacts of climate change, vulnerable populations, environmental justice, and strategies for adaptation, mitigation, and resilience in nursing.
- Collaboration with healthcare, public health, and advocacy groups to promote policies and initiatives based on principles of environmental justice and that address social inequities.
- Policy makers have evidence-based information to connect climate change with women’s health.
- Research progresses to provide more information on the associations between gender and health risks related to climate change and effective adaptation and mitigation strategies.
Box: Select climate change and health terminology3,4,6,10,19
- Adaptation: preparations that are made to blunt the disruptive impact of climate change and reduce vulnerability to its harmful effects
- Adaptive capacity: the ability of people, institutions, and communities to adjust to potential hazards, take advantage of opportunities, and respond to consequences
- Climate change: changes in the state of the climate attributed directly or indirectly to human activity that alter the composition of the global atmosphere and that persist over time
- Exposure pathways: routes through which people are exposed to climate change impacts that can affect human health
- Fine particulate matter: small-sized particulate air pollutants produced by burning fossil fuels that are easily inhaled into the lungs
- Fossil fuels: hydrocarbon fuels (eg, petroleum, coal, natural gas) derived from the accumulated remains of prehistoric plants and animals in the earth’s crust. Carbon dioxide and other greenhouse gases are generated from burning fossil fuels.
- Greenhouse gases: gases such as carbon dioxide, nitrous oxide, methane that absorb and re-emit heat acting as insulators that increase the temperature of the earth’s atmosphere
- Ground-level ozone: chemicals produced by burning fossil fuels trapped in the atmosphere commonly referred to as smog
- Mitigation: efforts to reduce the underlying causes of climate change and thus prevent continued damage to the life-sustaining systems that support human life
- Resilience: ability to prepare and plan for, absorb, recover from, and more successfully adapt to adverse events
- Vulnerability: tendency or predisposition to be adversely affected by climate-related health effects
References
- World Health Organization. Gender, Climate Change and Health. 2014. www.who.int/globalchange/ GenderClimateChangeHealthfinal.pdf.
- Sorensen C, Murray V, Lemery J, Balbus J. Climate change and women’s health: impacts and policy directions. PLoS Med. 2018;15(7):e100603.
- International Council of Nurses. Position Statement: Nurses, climate change and health. 2018. www.icn.ch/sites/default/files/inline-files/ ICN%20PS%20Nurses252c%20climate%20change%20and%20 health%20FINAL%20.pdf.
- Sarfaty M. Climate Change and Population Health: A Primer. Burlington, MA: Jones & Bartlett Learning; 2020.
- World Health Organization. Climate change and health. February 1, 2018. www.who.int/news-room/fact-sheets/detail/climate-change- and-health.
- Allen PJ. Climate change: a review of potential health consequences. Primary Health Care. 2015;25(7):34-40.
- Dodgen D, Donato D, Kelly N, et al. 8. Mental health and well-being.The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. Washington, DC: US Global Change Research Program, 2016; 217-246.
- Olson DM, Metz GAS. Climate change is a major stressor causing poor pregnancy outcomes and child development. F1000Res. 2020;9:F1000 Faculty Rev-1222.
- Nicholas PK, Breakey S. Climate change, climate justice, and environmental health: implications for the nursing profession. J Nurs Scholarsh. 2017;49(6):606-616.
- Gamble JL, Balbus J, Berger M, et al. 9. Populations of concern. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. Washington, DC: US Global Change Research Program, 2016; 247-286.
- van Daalen K, Jung L, Dhatt R, Phelan AL. Climate change and gender-based health disparities. Lancet Planet Health. 2020;4(2):e44-e45.
- Watts N, Amann M, Arnell N, et al. The 2020 report of the Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397(10269):129-170.
13. Whitehead L. The road towards environmental justice from a multifaceted lens. J Environ Health. 2015;77(6):106-108.
14. Mary Robinson Foundation Climate Justice. Future Generations. www.mrfcj.org/our-work/areas-of-work/future-generations.
15. International Federation of Obstetrics and Gynecology. Climate crisis and health. April 2020. https://www.figo.org/news/statement- climate-crisis-and-health.
16. United Nations Climate Change. Introduction to gender and climate change. 2021. https://unfccc.int/gender.
17. Kuehn L, McCormick S. Heat exposure and maternal health in the face of climate change. Int J Environ Res Public Health. 2017;14(8):853.
18. Bekkar B, Pacheco S, Basu R, DeNicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3(6): e208243.
19. ecoAmerica. Let’s Talk Health & Climate: Communication Guidance for Health Professionals. Washington, DC: Climate for Health; 2016.
20. Leffers J, McDermott Levy R, Nicholas PK, Sweeney CF. Mandate for the nursing profession to address climate change through nursing education. J Nurs Scholarsh. 2017;49(6):679-687.
21. Alliance of Nurses for Healthy Environments. Nursing collaborative on climate change and health. April 14, 2017. www.envirn.org/ nursing-collaborative.
22. American College of Nurse-Midwives. Position Statement. Climate change and maternal, fetal, and infant health. May 2017. ClimateChangeMaternalFetalInfantHealthMay2017.pdf.
23. American Nurses Association. Resolution. Global climate change. 2008. www.nursingworld.org/~4afb0e/globalassets/ practiceandpolicy/work-environment/health–safety/global- climate-change-final.pdf.
24. Canadian Nurses Association. Position statement: climate change and health. June 2017. www.cna-aiic.ca/~/media/cna/page-content/pdf-en/climate- change-and-health-position-statement.pdf.
25. Leffers J, Butterfield P. Nurses play essential roles in reducing health problems due to climate change. Nurs Outlook. 2018;66(2):210-213.
APPROVED BY NPWH BOARD OF DIRECTORS: JUNE 11, 2021

