Black Women Show Even Greater Benefit, AHA Journal Study Finds
pregnancy
Advice for Pregnant, Nursing Women Considering a COVID Vaccine
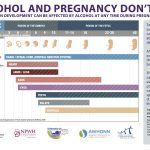
Alcohol Free Holidays for Baby and Me
Breastfeeding complications in a Filipino American patient
Case Study: Acute Abdominal Pain at 31 Weeks’ Gestation
Conservative measures to manage acute appendicitis without surgery can be an acceptable choice for pregnant women meeting appropriate criteria.
Clinical Topics: Prenatal and Postpartum
Clostridioides difficile in pregnancy
CMV virus is way more common than Zika. But expectant mothers don’t know their babies are at risk.
Collaborative care in a rural setting for a pregnant woman with heroin addiction
Covid Vaccine Doesn’t Reduce Conception Odds, But Getting Covid Does
Couples who get vaccinated against Covid do not reduce their chances of conceiving a child, but men who get infected with Covid do reduce their odds slightly.
Current recommendations for screening and management of postpartum depression
Debate Over Use of Blood Thinners After C-Sections
There’s sharp debate about whether the wide use of heparin to prevent clots in mothers after a C-section is effective, worth the cost and safe, since it carries the risk of bleeding.
Disproving Penicillin Allergy in Low-Risk Pregnant Women
New Data on Safety—and Best Reasons to Advocate De-labeling
Drugs in pregnancy, lactation, and reproductive health: Standards for prescribers
FDA Panel Backs Pfizer RSV Vaccine for Pregnant Patients
Fears surrounding pregnancy and motherhood among women with cystic fibrosis
Fertility preservation for young cervical cancer survivors
Freezing Ovarian Tissue May Be a Promising Fertility Treatment
Hypothyroidism in pregnancy
Immunizations for pregnant persons: Current recommendations for clinical practice
Implementation of the Maternal Mental Health Safety Bundle: Standardizing perinatal depression screening and response in a federally qualified health center
A national survey of obstetricians and gynecologists reported that 53% universally screened pregnant patients for depression, but only 33.67% implemented guideline-congruent care.
Improving prenatal health behaviors: Implementing a blended model of prenatal care
Infants Can’t Get Covid-19 Vaccine, But Their Moms Should: CDC
Low-Dose Aspirin May Improve Pregnancy Odds
Women who have had one or two miscarriages may improve their chances of pregnancy and live births by taking a low-dose aspirin.
Managing the sugar blues: Putting the latest gestational diabetes mellitus guidelines into practice
Marijuana use may hurt chances of getting pregnant, study suggests
The Effects of Cannabinoids on Women’s Reproductive Health, including fertility, will be the focus of a breakout session at the 24th Annual NPWH Premier Women’s Health Conference to be held Oct. 13-16
New Diabetes Guidelines Impact Screening, Pregnancy
Nurse Midwives Step Up to Provide Prenatal Care After Two Rural Hospitals Shutter Birthing Centers
Midwives can provide many other types of care for women and for babies.
Perinatal anxiety disorders: Assessment and management
Peripartum Cardiomyopathy: Implications for WHNPs and Midwives
In the US, the incidence of PPCM is rising, possibly due to advanced maternal age, an increased rate of multifetal pregnancies secondary to modern fertility techniques, and increased recognition and awareness of the disease.
Pregnant Women With Covid Pass Antibodies to Babies, Study Finds
Pregnant women who contract Covid-19 pass protective antibodies to their newborns. A Covid vaccine early in their pregnancy might do the same.
Prevention of Alcohol-Exposed Pregnancies
All sexually active women of reproductive age who could become pregnant and who drink alcohol need to be counseled about the potentially harmful effects of alcohol on a developing fetus.
Prior Migraines May Mean Riskier Pregnancy
Progesterone to Prevent Preterm Birth Effective Only in Women with Short Cervix, Study Finds
Providing Bias-informed and Evidence-based Care for Pregnant Persons with Obesity
Providing culturally sensitive evidence-based care for Orthodox Jewish women
Reassurance for Your Pregnant Patients on Antidepressants, Study Shows
Antidepressant Use During Pregnancy Does Not Raise Risk of Neurodevelopmental Disorders in Children
Researchers provide new insights into age-related female infertility
Researchers Say Coronavirus Does Not Appear To Pass From Pregnant Women To Infants
Rural Hospitals Weigh Keeping Obstetric Units When Births Decline
Just 7.4% of U.S. babies are born at hospitals that handle 10 to 500 births annually but those hospitals are 37% of all U.S. hospitals that deliver babies.
Rush for Covid Vaccines Left the Pregnant Behind
“Our failure as a society to vaccinate women in pregnancy will be remembered by the children and families who lost their mothers to this disease.”
Shorter Hospital Stays, Milder Illness for Breastfed Babies
First Study to Measure Breastfeeding Effect on Disease Prognosis, Duration of Hospitalization
Some Caffeine During Pregnancy Not Only Safe, But Helpful
Having 100 mg of caffeine a day during pregnancy not only doesn’t increase the risk of preeclampsia or hypertension, but it may lower the risk of gestational diabetes.
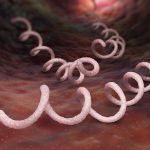
Syphilis update for women’s healthcare providers
Treatment Offers Fertility Hope for Early Menopausal Women
A small study suggests platelet-rich plasma and gonadotropins may help restore fertility in women who entered early menopause but want to become pregnant.
Update on perinatal anxiety disorders: Assessment and management
USPSTF: Screen All Pregnant Women for Pre-eclampsia
Vaccination Against COVID-19 Supports a Healthy Pregnancy by Protecting Both Mother and Child
COVID-19 poses a significant threat to both the mother and child, and vaccination can help mitigate that risk.