Shifting toward remote screening means primary care providers who work in rural, low-income and other marginalized communities could conduct medication abortion screening and increase equitable access to abortion care.
reproductive health
Assessment and Management of PMS and PMDD in the Adolescent
Discussing menstrual cycle-related mood symptoms provides an opportune time during the visit to complete depression screening.
Biden Health Pick Must Tread Carefully on Abortion, Family Planning
Clinics and women’s health advocates want to unwind Trump-era funding cuts and rules that decimated reproductive health providers.
Challenges of preconception and interconception care: Environmental toxic exposures
Clinical Topics: Reproductive and Sexual Health
Current barriers to LARC removal: Threats to reproductive autonomy
Developing and implementing PrEP at your local health center
Drugs in pregnancy, lactation, and reproductive health: Standards for prescribers
Fears surrounding pregnancy and motherhood among women with cystic fibrosis
Online Data Could Be Used Against People Seeking Abortions if Roe v. Wade falls
Anyone in a state where abortion becomes illegal who relies on the internet for information, products and services related to reproductive health would be subject to online policing.
Practitioners Trying to Prescribe Abortion Pills Across State Lines Stymied by Legislation
Nurse practitioners who are getting licensed in multiple states so they can use telemedicine and mail-order pharmacies to help more women get medication abortions are being stymied by state regulations.
Seeing our invisible patients: The importance of providing inclusive sexual and reproductive healthcare to LGBTQ populations
We are Title X
Welcome to the Clinician Café—A unique learning model
What is Sexual and Reproductive Health Equity and Why Does it Matter for Nurse Practitioners?
To fully meet patients’ needs, provide compassionate care that helps our patients thrive, and to create the best health outcomes possible, it is important to make SRHE a priority in our practice.
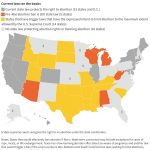
What’s Next if ‘Roe v. Wade’ Falls? More Than Half of States Expected to Ban or Restrict Abortion
If the Supreme Court overturns Roe v. Wade, the effects would be sweeping for 40 million women in more than two dozen states.